José de Jesús Alba-Romero1,2*, Graciela Castro-Escarpulli3, Damari L Alba-Romero2, Rebeca Pérez-Morales1, Yasmín Calleros-Rincon1 and Gloria G Guerrero4*
1División de Estudios de Postgrado e Investigación, Facultad de Ciencias Químicas, Unidad Gómez Palacio, Universidad Juárez del Estado de Durango, Gómez Palacio, Durango, México
2Laboratorio de Análisis Clínicos Asesores Especializados de La Laguna, Gómez Palacio, Durango, México
3Escuela Nacional de Ciencias Biológicas del IPN, CDAD de México, México
4Unidad Académica de Ciencias Biológicas, Universidad Autónoma de Zacatecas, Zacatecas, Zac, Mexico
*Corresponding Author: José de Jesús Alba-Romero, División de Estudios de Postgrado e Investigación, Facultad de Ciencias Químicas, Unidad Gómez Palacio, Universidad Juárez del Estado de Durango, Gómez Palacio, Durango, México and Gloria G Guerrero, Unidad Académica de Ciencias Biológicas, Universidad Autónoma de Zacatecas, Zacatecas, Zac, Mexico.
Received: August 19, 2024; Published: September 17, 2024
Citation: José de Jesús Alba-Romero., et al. “First Case of Pulmonary Lophomoniasis in a Daycare Child in Northern Mexico: A Clinical Report". Acta Scientific Microbiology 7.10 (2024):44-48.
Pulmonary lophomoniasis is a respiratory syndrome, poorly known disease in Mexico and worldwide, which makes diagnostic and treatment very difficult. In a previous work we have reported that lophomoniasis diagnostic in adults can be carried out using microbiological techniques correlating the presence of Lophomonas blattarun by observation of the movement of trophozoites and with Gram staining. Herein, we are presenting a clinical case of a 4-year-old female pediatric patient with diagnosis and treatment for bronchial asthma since she was 2 years old. The patient evolved into respiratory syndrome with productive cough and in recent weeks developed fever. A fresh study of BAL was carried out under an optical microscope observing morphological structures corresponding to Lophomonas blattarum (L. blattarum), trophozoites, Gram staining was also performed. Pseumodomonas aerugionosa and moderate development of Candida albicans were isolated in the cultures. After metronidazole treatment for 10 days the cough subsided completely and there was no fever. However it is important to known that L. blattarum is a pathogenic agent of the respiratory tract of immunosuppressed patients of all ages and sanitary measures should not be disregarded.
Keywords: Lophomonas blattarum; Lophomoniasis; Respiratory Syndrome
Bronchopulmonary lophomoniasis (LBP) is a rare and potentially fatal disease that affects patients of all ages, most frequently in Asian and Latin American countries [1]. However, in Mexico only one case of bronchopulmonary lophomoniasis (BLP) has been described in a child after he was transplanted, is a protozoan lung disease that has been reported sporadically, but its incidence has been increasing. However, the epidemiology and risk factors of the disease have not been clearly identified [2].
Lophomonas sp. It is a common parasite of the intestinal tract of cockroaches and is not recognized as a pathogen for humans. However, there are few reports of lophomonas in respiratory tract secretions in patients with severe lung disease, mainly in adults [3]. Protozoal infection is always associated with individual states of suppressed immunity, which can be caused by acquired immunodeficiency syndrome (AIDS), transplants, malignant blood diseases and corticosteroid therapy. Visiting endemic areas, having pets, and exposure to a dirty environment could also increase the chance of contracting the disease [4]. The diagnostic is not easy because parasitic lung infections, including protozoan and helminth infections and can be confused with problems of bronchial asthma, allergies and often with tuberculosis. Furthermore, the lack of information about this protozoan is the lack of knowledge of the pathophysiology, the morphology which has been confused with macrophages in many cases and most importantly, that diagnostic laboratory personnel do not identify them [5].
blattarum is a rare multiflagellate protozoan, it can affect the lungs, maxillary sinuses and genitourinary tract, infected patients present nonspecific symptoms such as fever, cough and dyspnea. Chronic respiratory symptoms with eosinophilia are often attributed to allergy, asthma, Loeffler syndrome, and filariasis. Some countries have reported cases of pulmonary lophomoniasis in children with similar symptoms such as an evolutionary period with chronic cough of more than 3 months, intermittent fever, eosinophilia in peripheral blood and in expectoration, high IgE levels, which makes the diagnosis confused [6]. In general the diagnosis is based on the identification of live forms of protozoa in fresh samples of respiratory secretions (bronchoalveolar lavage) [7]. which is routinely performed in adults to take samples of cellular and biochemical components. On the contrary, despite a global increase in the use of BAL in children, including newborns, there are no clear recommendations on the methodology [8]. In addition, reports of infections predominantly in immunocompromised individuals may be biased due to more invasive procedures to establish the etiological diagnosis of respiratory symptoms that do not resolve [9].
A 4-year-old female pediatric child for approximately 6 months. It is managed with a conventional diagnosis and treatment for bronchial asthma because she sporadically presented wheezing, the patient has been in day care since she was 18 months old and in the last 6 months she has had frequent cough, productive cough and in the last two weeks It evolved into respiratory syndrome, with a productive cough and in recent weeks he developed fever.
Blood count with leukocytosis 12.9 x103/µL, with a differential of 78% polymorphonuclear cells, monocytes 4%, eosinophils 8%, basophils 2%, lymphocytes 8%. Glucose 78%, Total Bilirubin 0.8 mg/dL, AST 30 IU, ALT 25 IU. General urine examination with leukocytes of 2-4/C. scarce bacteria and normal urinary chemistry. A tele chest x-ray was requested, finding congestion in both lungs. In addition, in the imaging results, the tree-in-bud sign was present, which is the non-specific tomographic manifestation of a disease of the small peripheral airway that causes dilation and has the lumen occupied by mucus, water or pus, frequently associated with peribronchiolar inflammation.
Bronchoalveolar lavage (BAL) was performed on a 4-year-old female pediatric patient. The samples obtained from the BAL were sent to the laboratory for analysis. Culture for bacteria and fungi, Gram stain, and concentration bacilloscopy with Ziehl Neelsen stain were performed. The samples were sown on Casman agar with blood, Mac Conkey agar and Biggy agar in a class IIA biosafety cabinet, they were incubated for 18 to 24 h at 36°C, the microorganisms were identified in the automated Vitek II Biomerieux VITEK® system. The 10% KOH test; The direct microscopic examination test was also carried out by placing 50 µL of BAL liquid with a drop of KOH, putting 50 µL of BAL liquid on slide, covered with copper glass.
Pseudomonas aeruginosa and Candida albicans were identified in BAL using the Vitek II Biomerieux VITEK® automated system. The KOH test was positive for yeasts and hyphae. The smear for acid-fast bacilli (BBAR) was negative. Gram staining demonstrates the presence of Gram-negative bacilli, few yeasts and structures that are compatible with ciliated and bronchoalveolar cells, as well as structures that correspond to Lophomonas spp (Figure 1). Furthermore, in the fresh microscope examination, protozoans morphologically compatible with Lophomonas blattarum and ciliated aveolar cells were observed, Figure 2.
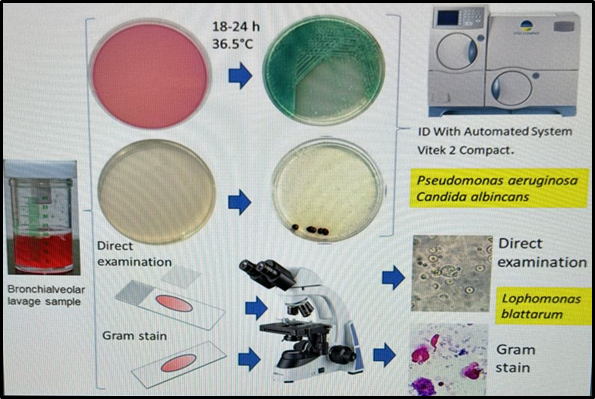
Figure 1: Scheme of the differential identification of different species of bacteria, fungi and parasites in BAL versus Lophomonas. Phenotypic identification for bacteria and fungi by the automated method of vitek 2 Compact. Identification of protozoans (L. blattarum) in direct microscopic examination. Identification of protozoans (L. blattarum) by Gram staining and observed microscopically.
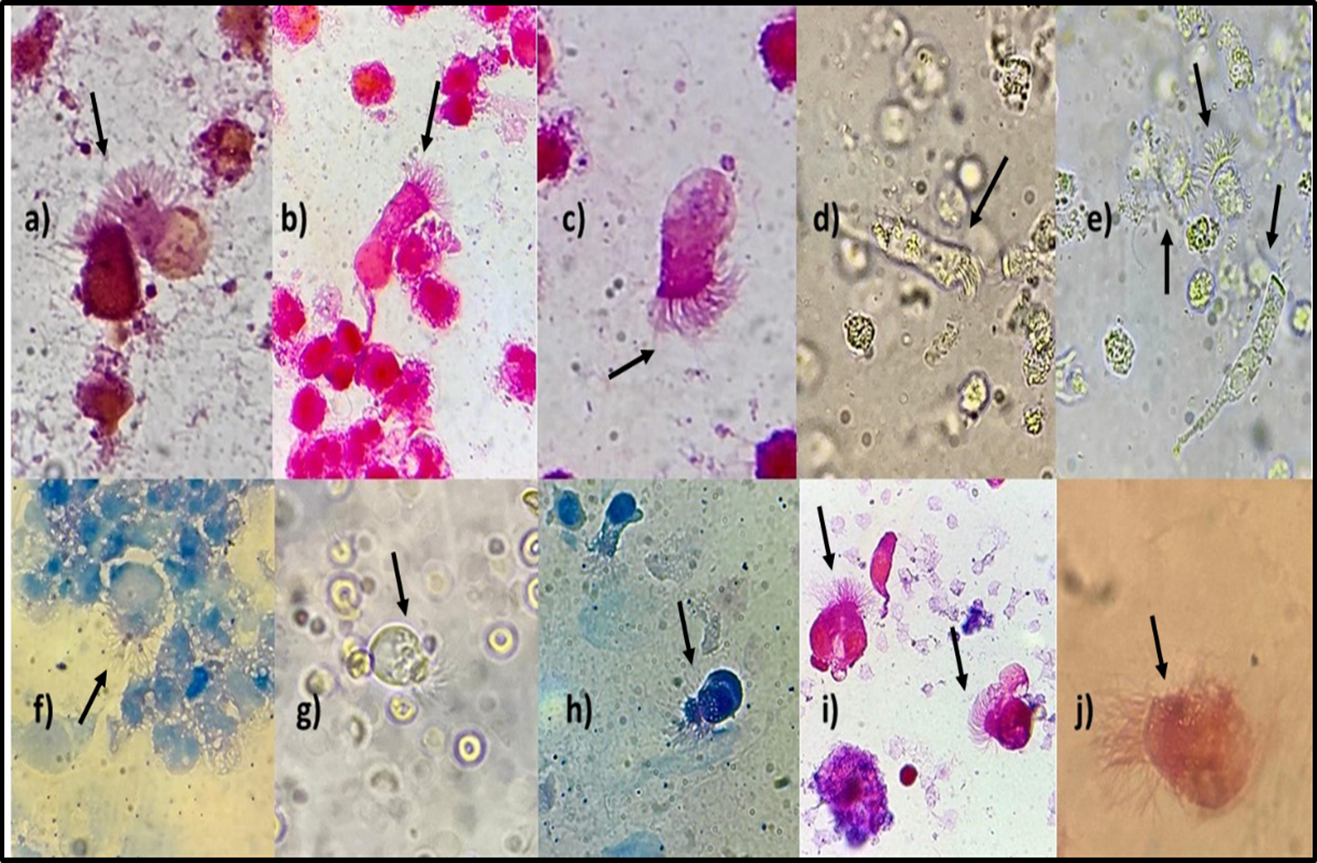
Figure 2: Identification and Analysis of Lophomonas blattarum with Gram Staining in the BAL of a child of four years old. a), b), c) Bronchoalveolar cells with Gram stain. d), e) Bronchoalveolar cells observed in 40X fresh examination. f), h), g) Lophomonas blattarum with Ziehl Neelsen stain. i) Lophomonas blattarum with Gram stain. j) Lophomonas blattarum observed in fresh 40X examination.
In the present study is reported for the first time the presence of Lophomonas blattarum in BAL of a four-years-old from a daycare Center in the North of Mexico. The initial clinic manifestation evolved into respiratory syndrome, with a productive cough and in recent weeks she developed fever. After pharmacological treatment the infection relapsed. Despite this, this study pinpointed that sanitary conditions, nutritional diets in Childs should be not disregarded, aiming to robust the immune system against any type of pathogens, like for example Lophomonas.
Chronic respiratory diseases (CKD) are among the leading causes of death and disability in the Region of the Americas. CKDs include chronic obstructive pulmonary disease (COPD), asthma, and other chronic respiratory diseases such as occupational lung diseases and pulmonary hypertension [10]. The study addressed the issue of CKD as those that affect the lungs can be caused by bacteria, fungi, parasites. This last one is represented by L. blattarum as a complex causal agent to diagnose [11]. To be successful in the diagnosis of pulmonary lophomoniasis, experience is required, especially in the morphological identification and differentiation of hair cells, otherwise an erroneous diagnosis may be given, as described by Ding Q and Shen k. (2021), a protozoan considered emerging globally after the COVID-19 pandemic, is Lophomonas blattarum [12]. The incidence of L. blattarum is increasing worldwide as described in previous publications [13,14].
The study presented, pulmonary lophomoniasis in children as a condition with diverse symptoms and that was confused with allergic processes, sinusitis, however, the persistent symptoms, fever and lack of response to treatment should be considered in a patient with pulmonary lophomoniasis in pediatric patients which coincides with what was described by Singhal T [15]. The contamination of surfaces in daycare centers with little or no hygiene, such as the daycare floor, becomes a risk factor for children who do not yet walk, even if they only move around by crawling, and who develop these symptoms, they must be attended to with the probable diagnosis of lophomoniasis as stated by Taheri A., et al. [16]. Herein, it is presented a fresh examination and Gram and Ziehl-Neelsen stains. The perspective is to be able to develop and approach molecularly the study of this parasite because the analogy in the clinical symptoms with COVID-19 and Tuberculosis infections Zerpa R., et al. [17]. The efficiency in timely diagnosis is still under development and is a challenge for future studies.
Pulmonary lophomoniasis is a problem that affects immunosuppressed patients and affects patients of all ages under three important conditions, such as immunosuppression, second, poorly hygienic conditions and third the presence of cockroaches in the home is a triggering factor such as in this case. In educational centers and daycare centers that have maternal services and children who do not yet walk, but move on floors contaminated by cockroach excreta, they are the main risk factor for acquiring pulmonary lophomoniasis in pediatric patients. Therefore, this clinical case encourages special attention in day care centers.
The authors acknowledge to the health personnel in the hospital for technical assistance in the recollection of BAL samples.
The study and all the procedures for medical research involving human subjects, including research on identifiable human material and data were performed under the principles of the Declaration of Helsinki, and approved by the ethic committee in Research.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review.
The authors declare no competing of interests.
Data will be shared following institutional guidelines. The review of the literature was based on search and data from Pubmed database without limitation to 2021.
The study did not receive funding from any dependence nor a grant. J,A.R. Conceptualization, methodology, writing and discussion. G.G.G. is Perfil Prodep (A program of the National Secretary of Education). The authors received a fellowship by the National System of Researchers (SNI-CONACYT). Mexico.
JJAR. Conceptualization, methodology, writing and discussion. G.G.G. writing, discussion of the data. A.L.D.L., C.R.E.Y, P.M.R. contributed to the analysis and discussion of the data.
Copyright: © 2024 José de Jesús Alba-Romero., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.