Onosakponome Evelyn Orevaoghene1*, Nyenke Clement Ugochukwu1, Roseanne Adah Ikpeama1, Ndifrekeabasi Itek Robinson2 and Obe Emmanuel Olube3
1Department of Medical Laboratory Science, Pamo University of Medical Sciences,
Port Harcourt, Nigeria
2Department of Medical Microbiology and Parasitology, Rivers State University,
Port Harcourt, Nigeria
3School of Life Science, Engineering and Environment, The University of Salford, UK
*Corresponding Author: Onosakponome Evelyn Orevaoghene, Department of Medical Laboratory Science, Pamo University of Medical Sciences, Port Harcourt, Nigeria.
Received: July 19, 2024; Published: September 12, 2024
Citation: Nyenke., et al. “Maternal and Infant Factors Associated with Malaria in Cord Blood in Rivers State University Teaching Hospital, Port Harcourt". Acta Scientific Microbiology 7.10 (2024):09-16.
Cord blood, the blood found in the placenta after delivery, contains numerous stem cells and congenital pathogens that can cause infections. Malaria is one of the most prevalent congenital infections worldwide, particularly in developing countries like Nigeria. This study evaluates the presence of malaria parasites in cord blood concerning maternal and child factors. Conducted on 180 cord blood samples collected in the labour ward, this random study received ethical approval from the Ethics Committee of the Rivers State Teaching Hospital, Port Harcourt. Samples were examined for malaria parasites using Giemsa-stained blood smears under light microscopy. Maternal and child factors were gathered through a structured questionnaire. The data analysis was performed using the Statistical Package for the Social Sciences (SPSS). The overall malaria prevalence was 21.1%. The study found that maternal age, education level, and occupation did not significantly influence malaria prevalence. However, the infection rate in cord blood was significantly associated with birth weight, with newborns weighing 1.6-2.5kg showing the highest prevalence of 26.1%. The high malaria prevalence in this study highlights the need for health campaigns, routine testing, and proper prophylaxis during antenatal care to reduce congenital malaria transmission.
Keywords: Statistical Package for the Social Sciences (SPSS); Cord Blood; Malaria
Cord blood is the blood contained in the placenta after delivery. It is known to contain lots of stem cells and congenital pathogens. Congenital pathogens are the causative agents of congenital infections. Congenital infections affect the unborn fetus or newborn infant. It is vertically transmitted from mother to child during pregnancy, breastfeeding or birth. Some examples of these congenital infections are malaria, toxoplasmosis, trypanosomiasis, syphilis, hepatitis B, rubella, herpes simplex virus, chagas, human immunodeficiency virus (HIV) [1]. Prevalence of congenital infection ranges from 0.1 to 0.3 per 1000 live births [2].
Malaria occurs primarily in tropical and subtropical countries. The vast majority of malaria cases and deaths are found in the African Region, with nearly all cases caused by the Plasmodium falciparum parasite, (WHO, 2023). This parasite is also dominant in other malaria hotspots, including the regions of South-East Asia, Eastern Mediterranean and Western Pacific. The threat of malaria is highest in sub-Saharan Africa, and 4 countries in that region accounted for nearly half of all malaria deaths worldwide in 2021: Nigeria (26.6%), the Democratic Republic of the Congo (12.3%), Uganda (5.1%), and Mozambique (4.1%) [3]. The infection can also spread congenitally to newborns from their mothers. Its major infection in pregnancy can cause spontaneous abortion, death shortly before or after birth, abnormal organ development in the fetus, contingent on the stage of the pregnancy [4]. Congenital malaria is defined as the demonstration of malaria parasites in the peripheral blood smear of a neonate from birth to day 7 of life [1,3]. The presence of malaria parasites in cord blood is a key indicator of congenital malaria. This condition occurs when malaria parasites are transmitted from the mother to the fetus through the placenta during pregnancy [5,6]. Cord blood parasitemia signifies that the fetus has been exposed to the malaria parasites while in the womb [6]. This exposure can lead to congenital malaria, which is diagnosed when these parasites are detected in the infant's blood within the first seven days of life. The presence of parasites in cord blood is often associated with placental malaria, which is a significant risk factor for congenital malaria.. Congenital malaria is a major public health problem, as this disease is a threat to pregnant women and their children, with up to 200,000 stillborn babies each year due to the presence of malaria during pregnancy [4,5]. In Africa annually, more than 30,000,000 pregnant women live in malaria-endemic areas. The prevalence of malaria during pregnancy varies from 5 to 40% in endemic areas. According to the latest report, there were an estimated 247 million cases and 619 000 deaths globally in 2021 [3,5,6]. It is widely believed that the placenta acts as an effective barrier preventing transfer of malaria parasites. However, even in the absence of congenital malaria, placental malaria significantly increase the risk of perinatal morbidity and mortality including low birth weight, intrauterine growth restriction, preterm labor and intrauterine fetal death [7]. Malaria in pregnancy is estimated to account for 100,000 neonatal deaths annually [8]. Maternal malaria can be prevented during pregnancy with intermittent presumptive treatment of malaria in pregnancy (IPTp) using sulfadoxine–pyrimethamine, and can reduce neonatal mortality by up to 61% [7,9].
This study was conducted in Rivers State University Teaching Hospital (RSUTH), formerly Braithwaite Memorial Specialist Hospital (BMSH). It is a Government-owned hospital, named after Eldred Curwen Braithwaite, a British doctor and a pioneer of surgery. RSUTH is located at latitude 4°46’49"N and longitude 7°0’50"E in Port Harcourt Local Government Area (LGA), in Old GRA, Rivers State. The hospital is ranked among the largest hospitals in the Niger Delta, Nigeria. People from other parts of Rivers State and beyond attend the RSUTH for specialist’s services.
A qualitative cross sectional design was adopted and one hundred and eighty cord blood samples randomly collected from labor ward and surgery ward at Rivers State University Teaching Hospital (RSUTH), Port Harcourt, Rivers State, Nigeria.
Ethical approval was sought from Rivers State University Teaching Hospital (RSUTH), Port Harcourt (RSUTH/REC/2022271). and the subjects involved in the research via written and /or a verbal consultation and approval.
Socio-demographic information and obstetric history was obtained from participants by the use of structured questionnaire. Following informed consent and strict adherence to utmost confidentiality of treatment of all information obtained as specified in the ethical clearance guidelines given for this study.
Cord blood samples were collected and stored in Ethylene Diamine Tetra Acetate bottles to prevent coagulation.: Blood films (thick and thin)were prepared, stained (using Giemsa stains) from the collected blood samples, and visualized using X100 objective power lens of a microscope to detect the forms of Plasmodium present [10]. Thick blood smears were used to quantify parasites [10].
Data obtained was entered into Microsoft Excel and analyzed using Statistical package for the social sciences (SPSS) version 25. Descriptive analysis including frequencies and percentages was used to describe the population and also to assess the prevalence of Toxoplasma gondii and malaria parasite. Chi-square test and Kappa (K) was used to investigate associations and Agreement respectively among categorical variables and infection data.
Figure 1 shows the overall prevalence malaria in cord blood in Port Harcourt. Out of a total of 180 specimens were received, 38 of the cord blood samples were infected with malaria parasite providing a prevalence of 21.1%. Pearson chi test was used to evaluate the prevalence of malaria in cord blood and was statistically significant (P=0.000).
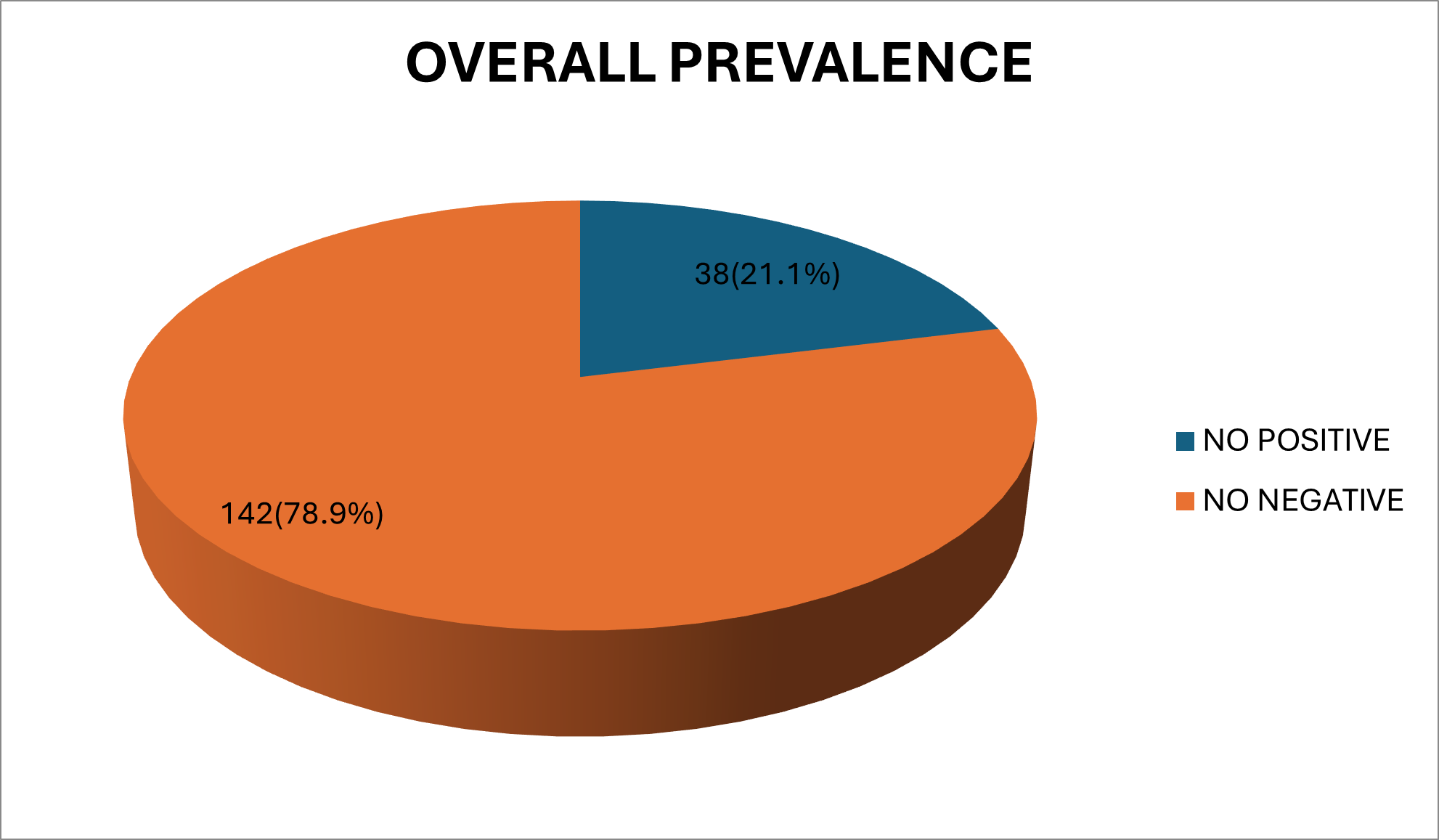
Figure 1: Overall prevalence of malaria in cord blood.
Table 1 shows the relationship of maternal factors and malaria in cord blood. The highest prevalence of malaria in cord blood was recorded in 18 mothers within the age range 26-35 years with a prevalence of 10%. Pearson chi test was used to evaluate the prevalence of malaria in cord blood and the relationship with maternal factors. The relationship between maternal factors and malaria was statistically insignificant.
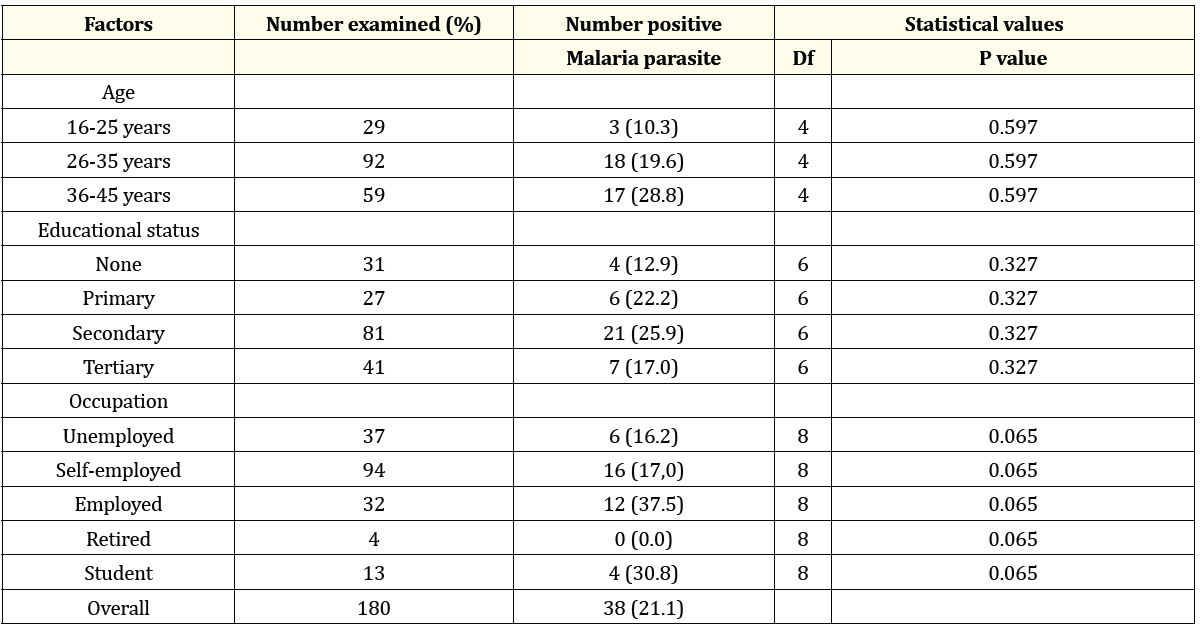
Table 1: Relationship of maternal factors and malaria in cord blood.
Table 3 shows the relationship of and newborn’s factors (sex and birth weight) and malaria in cord blood. The highest prevalence of malaria in cord blood was recorded in males with a prevalence of 39.4% and newborns with low birth weight within the range of 1.6-2.5kg with a prevalence of 37.8%. Pearson chi test was used to evaluate the prevalence of malaria in cord blood and the relationship with newborn’s sex and birth weight and was statistically insignificant for sex of newborn and malaria (P=0.736) and significant for birth weight of newborn and malaria (0.003).
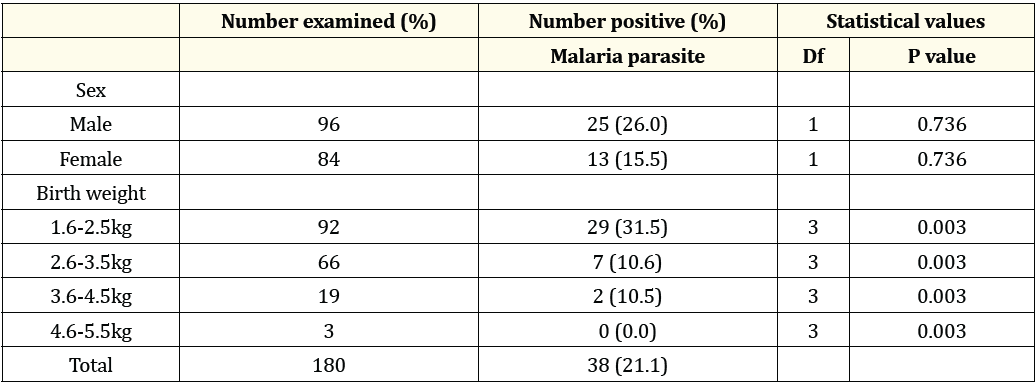
Table 2: Relationship between newborn’s factors and malaria in cord blood.
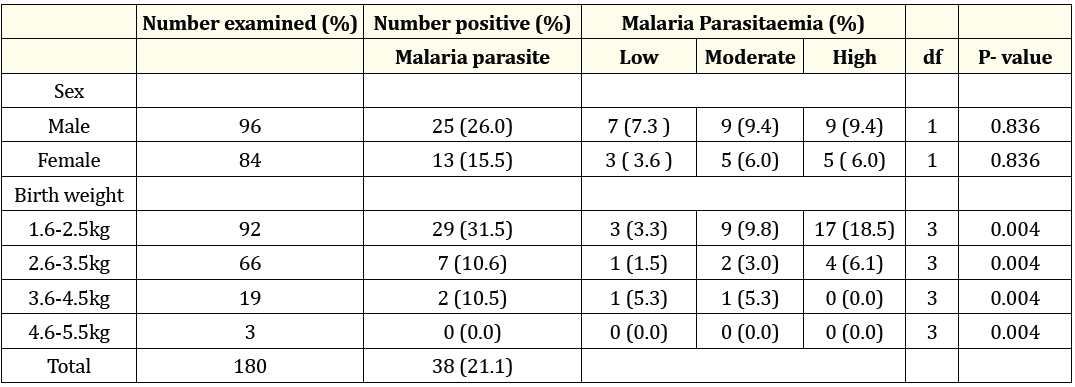
Table 3: Relationship between parasite intensity a Neonatal factors.
Malaria is a significant cause of congenital infections, posing serious risks to pregnant women, fetuses, and newborns. This study evaluated the prevalence of malaria in relation to maternal factors (age, education, and occupation) and child factors (sex and birth weight). A significant malaria parasitaemia level (21.1%) (p < 0.05) was found, likely due to the endemic nature of malaria in the study area, poor environmental sanitation, lifestyle factors, and misuse of antimalarial medications. Similar studies by Okoro., et al. (2022) and Tahirou., et al. (2017) reported prevalences of 21.72% in Owerri,Nigeria and 20.51%, in Niamey, Niger respectively. [11,12]. In contrast, Omalu., et al. (2012) in study in Minna, North Central Nigeria, observed a lower prevalence of 5.92% in cord blood parasitemia [13], Stephenson., et al. (2014), Bilal., et al. (2020) and Cardona-Arias., et al. (2022), with rates of 5%, in coastal Ghana, 16.2% in Columbia and 16.2% and respectively [13,14]. Another study in Jos, Nigeria, reported a higher prevalence of 33.6% for malaria parasites in cord blood [16]. These differences may be attributed to geographic location and prevailing sanitary and cultural practices.
This study found no significant association between maternal age and malaria infection in cord blood. However, Tahirou., et al. (2020) established a significant association in a similar study, potentially due to differences in testing methods, demographics, or geographic distribution [12].
The prevalence of malaria in cord blood concerning maternal education was not significant, although the highest prevalence was in mothers with up to basic education (secondary school). This may be due to lower disease awareness and greater environmental exposure.
Previous research by Omalu., et al. (2012) and okoro., et al. (2022) indicated that low birth weight is associated with congenital malaria [11,13]. This study also found that low birth weight (1.6-2.5kg) was linked to congenital malaria, with a prevalence of 26.1% with majority recording high parasitaemia level This suggests that malaria in cord blood impacts newborn weight. Studies have consistently shown that low birth weight is a major risk factor for higher malaria susceptibility, possibly due to weaker immunity and underdeveloped organs [11,13]. The distribution of parasitemia intensity in this present study shows that and a significant portion of high parasitemia (18.5%) is associated with low birth weight . this observation aligns with other findings where low birth weight was reported to be associated with higher malaria intensity, which can increase the risk of complications in newborns [12,13]. The lowest prevalence and absence of high parasitemia was observed in neonates within birth weight range 3.6kg – 4.5kg . This may invariably suggest that normal birth weight confers some protection against malaria, possibly due to a better-developed immune function compared to neonates with low birth weight [11-13].
The study highlights the significant prevalence of malaria in cord blood, with low birth weight being a critical factor. Maternal age, education, occupation, and newborn sex were not significantly associated with malaria prevalence. Routine comprehensive screening for pregnant women is recommended for early detection and management of malaria. Health campaigns should be conducted to raise awareness among medical personnel and patients about the infection.
The data you provided on the prevalence and intensity of malaria parasitemia in cord blood shows notable patterns when examined against sex and birth weight. Comparing these findings with existing literature reveals important insights.
Copyright: © 2024 Onosakponome Evelyn Orevaoghene., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.