Omorogbe Owen Stephen1*, Amegor Ilelosa Rock1, Obazee Osazee Toyin2 and Stanley Udogadi Nwawuba3
1Edo State Health Insurance Commission, Edo State, Nigeria
2Department of Family Medicine, University of Benin Teaching Hospital, Benin City, Nigeria
3Centre for Forensic Programmes and DNA Studies, University of Benin, Nigeria
*Corresponding Author: Omorogbe Owen Stephen, Edo State Health Insurance Commission, Edo State, Nigeria.
Received: June 03, 2024; Published: August 26, 2024
Citation: Omorogbe Owen Stephen., et al. “Factors Affecting Healthcare Utilization Among Edo State Civil Servants Enrolled on the Edo State Health Insurance Scheme". Acta Scientific Microbiology 7.9 (2024):34-41.
The population's health status is improved when healthcare is used effectively, and it is widely recognized that the mere existence of health facilities does not ensure that they will be used, as other socioeconomic factors may affect access and, consequently, utilization. Therefore, monitoring and evaluating healthcare provision and factors affecting healthcare utilization has become extremely necessary to improve the effectiveness of healthcare programs. In the light of this, the present study examined the factors affecting healthcare utilization among Edo State Civil Servants enrolled on the Edo State Health Insurance Scheme (EDOHIS). The design used in this study was the survey research design; descriptive statistics which involves the use of frequency and percentage was used for the analysis of 1000 questionnaires. The result revealed that majority of the participants were male (52.40%), 65.41% were married, it was observed that the age bracket 36-41years were the dominant population with 30.50%, a greater number of the participants 22.48% had 10-12 years of service, as per the educational status, 82.71% of the participants obtained a tertiary education and a greater proportion of the participants 49.07% had 4-6 persons as the household size. Participants responses on factors affecting healthcare utilization among Edo State Civil Servants enrolled on the Edo state Health Insurance Scheme revealed the following; as per the question, Are you aware of the details of your insurance health plan and benefit package? It was observed that majority of the enrolees reported yes (56%). A large proportion of the enrolees 61.1% reported that proximity and accessibility of assigned facility to address/workplace was an important factor in seeking care at the facility, 57.7% agreed that the prompt attention of the staff at the facility was an important factor regarding their continued patronage, 57.6% agreed that the availability of drugs at the facility was an important factor regarding the continued patronage, similarly 55.9% agreed that the type of illness is an important factor regarding their choice of seeking health care, and 66.1% agreed that the mode of payment/co-payment (10% for drugs and investigation was an important factor regarding their choice of seeking health care under the scheme. Finally, significant improvements can be made to the EDOHIS and Nigeria's larger healthcare system by focusing on specific domains including wait times, the attitude of healthcare professionals at the facility, laboratory and pharmacy services, and the full package of services supplied on health schemes.
Keywords: Factors Affecting Healthcare Utilization; Edo State Health Insurance Scheme; National Health Insurance Scheme, and Social Health Insurance Scheme in Nigeria
The World Health Organization defines universal health coverage (UHC) as a method of planning, providing, and financing health services so that "all people can access the health care they require without experiencing financial hardship" [1]. It offers financial protection from healthcare costs, especially during the time of service delivery, and first covers everyone with a package of high-quality essential health services [2]. The definition of UHC includes the objective of protecting individuals from monetary hardship and social injustice [1,3]. Social health insurance (SHI) is one of the possible organizational mechanisms for obtaining and pooling funds to support health care, alongside taxation, private health insurance, community insurance, and others [4]. By lowering catastrophic medical costs and pooling resources to enable cross-subsidization between the wealthy and the poor as well as between the healthy and the ill, it improves access to healthcare [1]. With the overarching objective of giving everyone the opportunity to sign up for at least one kind of mechanism that permits financial risks to be shared, such schemes have developed over time to reflect a variety of funding mechanisms, both voluntary and involuntary [5].
Additionally, households all over the world continue to experience tremendous hardship due to poor access to healthcare and the high expense of healthcare. According to a study by Nwanaji-Enwerem., et al. [6] over 930 million people spend 10% or more of their household income on healthcare services, and about 100 million people are pushed into extreme poverty as a result of medical expenses. Healthcare funding refers to methods for covering medical costs. Given that the final goal is to achieve predicted levels of health status and economic progress, any economy must provide appropriate money for health in order to grow [7,8].
The WHO encouraged member states to introduce either mandated health insurance, more equitable tax systems, or a combination of both in order to reduce direct payments and user fees for health services [9]. Around the turn of the century, many African nations began putting these ideas into practice. National health insurance plans (NHIS) were created in some countries and funded by taxes and insurance premiums. Certain disadvantaged populations or priority health services were not charged for by some [6,10]. According to Ahmed and Aliyu [11], Nigeria has one of the lowest health indices and highest out-of-pocket medical costs in the world. Financial risk management is required during illness in Nigeria because a large amount of health spending goes into out-of-pocket medical expenses, which prevents fair access to high-quality healthcare [12]. One such policy is the National Health Insurance Scheme (NHIS), whose main goal is to guarantee that it covers all Nigerians nationwide with the intention of providing a comprehensive and reasonably priced healthcare system [13-15].
The population's health status is improved when health services are used effectively. Studies have demonstrated that the mere existence of health facilities does not ensure that they will be used, as other socioeconomic factors which is a multidimensional construct comprising multiple factors, such as income, education, employment status, and other factors may affect access and, consequently, utilization [7]. Similar to this, low health facility utilization frequently reflects subpar treatment and unfriendly staff [16,17]. Insurance is frequently reported to increase utilization and reduce out-of-pocket (OOP) spending. Research has also shown that the NHIS is underutilized in Nigeria due to inadequate coverage nationwide, low health-seeking behavior among Nigerians, accessibility to healthcare facilities, length of wait times for services, and lack of key medications [15,18,19]. The NHIS and health management organizations (HMOs) have been actively advocating for and raising awareness of the health insurance program, yet it is commonly acknowledged that this program is still not frequently used by the public [20,21]. Therefore, monitoring, evaluating and assessment of factors that affect the utilization of healthcare services have become necessary to improve future implementation strategies.
A list of all health care facilities within the study area; was obtained from the Edo State Ministry of Health. Next, a list of all Edo State Health Insurance Scheme (EDOHIS) accredited facilities was obtained from the Edo State Health Insurance Scheme in Benin. As, for the choice of enrolees, sixty-four ministries, departments and agencies (MDAs) were selected. The selected facilities were visited and the number of enrolees in each of the selected health facilities was verified. Proportionate allocation of the estimated sample size (1000) was done based on the number of enrolees across the selected EDOHIS accredited facilities. All selected healthcare facilities were secondary level facilities (public, private non-faith-based, and private faith-based). Data collection spanned 2 months.
A list of EDOHIS enrolees waiting to receive care in the outpatient section of a selected health facility was obtained from the medical records department of the facility. Eligible individuals were the principal enrolees or spouses (excluding dependents under the age of 18 years) and had enrolled in the facility for at least 1 year before the commencement of the study. This was to increase the possibility that study participants had an appreciable level of interaction with the health system under the scheme that will enable appropriate responses from them. Among this population, enrolees who began using the selected facilities before the commencement of the health insurance scheme were excluded from the study as well as enrolees who were health care workers in the selected facilities. The total number of eligible individuals present in the clinic was used to generate a sampling frame. A sampling interval was determined, and systematic random sampling was used to select eligible participants. Systematic sampling was chosen because it eliminates the phenomenon of clustered selection and has a low probability of data contamination. The disadvantage of using a systematic sampling technique is noted and is considered a study limitation. The hospital card numbers of the enrolees who were used as participants were documented and kept safe.
For this research work, the research instrument adopted was a formal standardized questionnaire. A total of 1000 questionnaires were distributed to enrolees in selected EDOHIS accredited facilities in Edo state. The questionnaire comprised of two main categories:
Respondents were informed of the purpose of the study. They were informed that their participation in the study was voluntary and not paid for. They were also informed that the information provided was strictly for research purposes, and were requested to kindly provide honest responses to ensure the credibility of the study.
The respondents were informed that their identity was confidential and as such their detail of names and picture were not collected.
Informed consent was obtained from all individual participants included in the study.
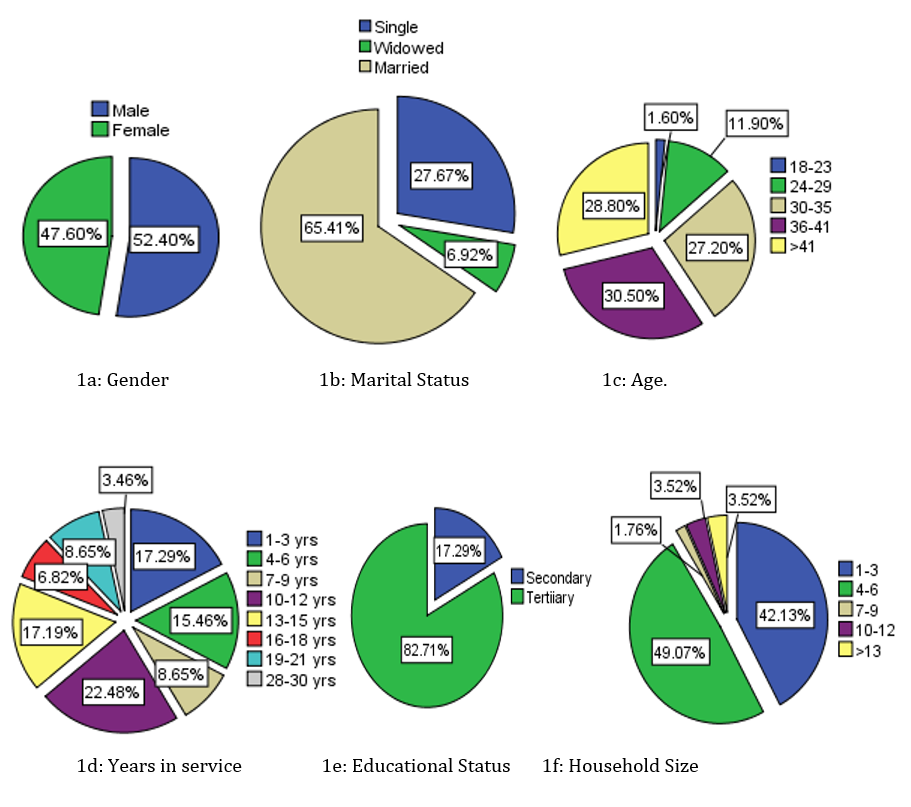
Figure 1: Showing Socio-demographic information of the participants.
Six variables representing socio-demographic information of the participants were examined, and the result revealed the following from a study population of one thousand participants; as per gender, it was observed that the majority of the participants were male (52.40%), the result on marital status shows that a greater proportion of the participants were married (65.41%) and the lesser number of the participants were widowed (6.92%), and for the variable age, it was observed the age bracket 36-41 years were the dominant population with 30.50%, followed by >41 (28.80%), then 30-35 (27.20%) and the age 18-23 was found to be the least participating population. Years in service of the participants were also examined and the result revealed that a greater number of the participants (22.48%) had 10-12 years of service. As per the educational status, 82.71% of the participants obtained a tertiary education and finally, the result of the household size of the participants revealed that a greater proportion of the participants 49.07% and 42.13% had 4-6 persons and 1-3 persons respectively as the household size.
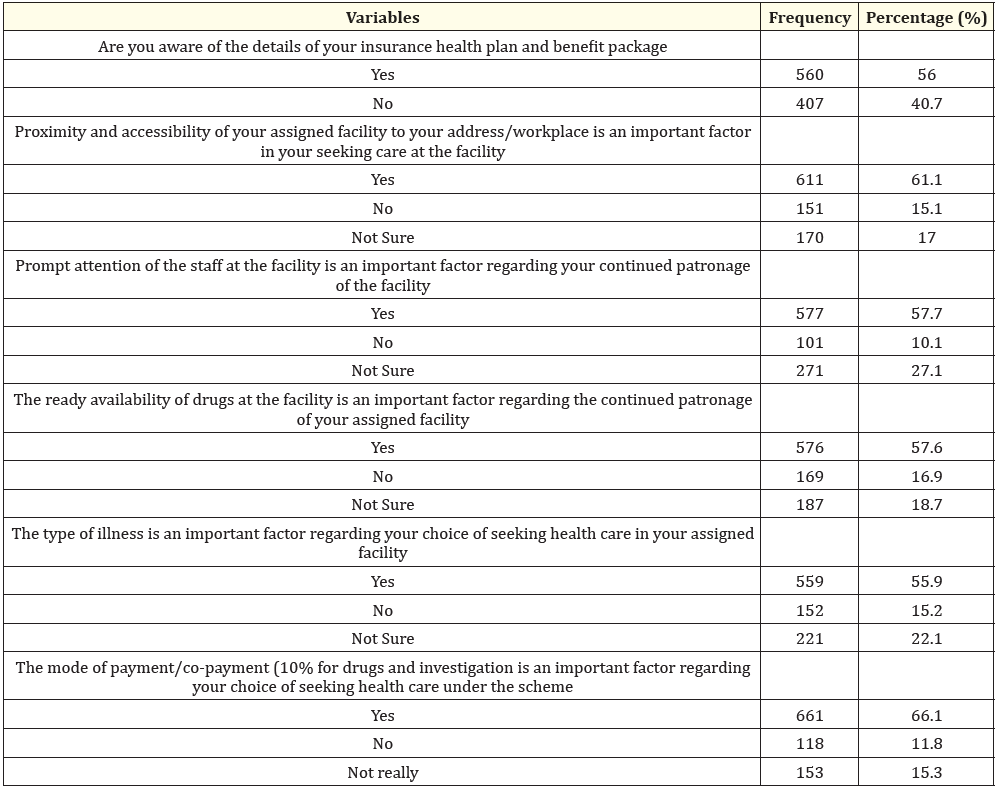
Table 1: Factors affecting healthcare utilization among Edo State Civil Servants enrolled on the Edo state Health Insurance Scheme.
Participants responses on factors affecting healthcare utilization among Edo State Civil Servants enrolled on the Edo state Health Insurance Scheme were collected and analyzed via a well-structured questionnaire and the result revealed the following; as per the question, Are you aware of the details of your insurance health plan and benefit package? It was observed that majority of the enrollees reported yes (56%). A large proportion of the enrollees 61.1% reported that proximity and accessibility of assigned facility to address/workplace was an important factor in seeking care at the facility, 57.7% agreed that the prompt attention of the staff at the facility was an important factor regarding continued patronage of the facility, 57.6% agreed that the ready availability of drugs at the facility was an important factor regarding the continued patronage of assigned facility, similarly 55.9% agreed that the type of illness is an important factor regarding their choice of seeking health care in assigned facility, and 66.1% agreed that the mode of payment/co-payment (10%) for drugs and investigation was an important factor regarding choice of seeking health care under the scheme.
In Nigeria, the underutilization of healthcare services varies from area to region and from state to state. It has also been noted that the health insurance program is still not widely used by the populace, necessitating ongoing efforts to change this [8,20,21]. The monitoring, evaluation, and assessment of health care provision and factors affecting healthcare utilization has become extremely necessary to improve implementation strategies, the effectiveness of healthcare programs, and the sustenance of the healthcare system [18,22,23]. In the light of this, the present study examined the factors affecting healthcare utilization among Edo State Civil Servants enrolled on the Edo State Health Insurance Scheme (EDOHIS). The result on the sociodemographic information of the participants revealed that a vast proportion of the participants were male indicating that enrollees of EDOHIS are predominantly males and this outcome maybe in part due to the fact that the benefits do not only cover for the enrollee but his entire household and as such it was observed that a greater proportion of the participants 49.07% had 4-6 persons as the household size. Clearly, the majority of the participants were noted to be married perhaps as a result of the expansive nature of the scheme, covering for the enrollee as well the household. Other variables were also examined. As per the age, it was observed the age bracket 36-41 were the dominant population with 30.50%; years in service of the participants were also examined and the result revealed that a greater number of the participants (22.48%) had 10-12 years of service, and as per the educational status, 82.71% of the participants obtained a tertiary education.
The National Health Act, which was passed into law in 2014, demonstrated Nigeria's commitment to reducing OOP and enhancing access to top-notch fundamental health services. It has been reported that the Nigerian healthcare system is currently undergoing significant reforms in health-care financing in order to achieve universal health coverage (UHC) [1,24]. Similar to this, the federal government of Nigeria has stated that all states must set up and maintain mandatory state health insurance systems [25]. Some states across the country have implemented state-wide health insurance plans for this reason [26]; with EDO state among the frontrunners with the establishment and implementation of Edo State Health Insurance scheme (EDOHIS). It has been extensively recognized that a number of factors influence the use of healthcare, including proximity and accessibility of the assigned facility, prompt staff response, the availability of pharmaceuticals at the facility, and the method of payment [15,27-29]. This widely reported factors that affect the utilization of healthcare schemes were examined for enrolees of EDOHIS and it was observed that the enrolees considered this factors as pointers to better utilization of the scheme. The findings of our study indicated that enrollees prefer facilities that are easy to reach, demonstrating that improving the geographic distribution of healthcare facilities can enhance access to care. This is particularly important for populations with mobility issues, limited transportation options, or time constraints due to work or family commitments. Delays and long waiting times can deter individuals from seeking care, potentially exacerbating health issues. Healthcare facilities should focus on streamlining their processes, improving staff efficiency, and managing patient flow to reduce waiting times and enhance patient experience. Similarly, the availability of necessary medications is critical for effective treatment and patient satisfaction and the severity and nature of an illness significantly influence healthcare-seeking behavior. Patients may prefer specialized facilities for certain conditions, or may seek immediate care for acute issues. Understanding the types of illnesses that drive healthcare utilization can help in tailoring services and resources to meet patient needs effectively. Additionally, financial considerations are a major determinant of healthcare access. The affordability of care, including the cost-sharing mechanisms, significantly impacts patients' decisions to seek care. A co-payment system that is perceived as fair and manageable encourages utilization. It is crucial to design payment models that minimize financial barriers while ensuring sustainability for the healthcare system. In comparison to similar study, currently, there are no existing studies on the factors affecting healthcare utilization among Edo State Civil Servants enrolled on the Edo state Health Insurance Scheme. However, similar studies were found in other states in Nigeria. A study conducted in Plateau State revealed that high cost of drugs, service charges, and the deprived attention of the staff at the facility were the major factors affecting the healthcare utilization in the state [17], and a similar finding was observed in another study conducted in southwest Nigeria [30].
Widely reported factors that affect the utilization of healthcare schemes were examined for enrolees of EDOHIS and it was observed that the enrolees considered these factors as pointers to better utilization of the scheme. It was observed that majority of the enrolees reported that proximity and accessibility of assigned facility to address/workplace was an important factor in seeking care at the facility, agreed that the prompt attention of the staff at the facility was an important factor regarding continued patronage, agreed that the ready availability of drugs at the facility was an important factor regarding the continued patronage, and agreed that the mode of payment/co-payment 10% for drugs and investigation was an important factor regarding choice of seeking health care under the scheme.
Copyright: © 2024 Omorogbe Owen Stephen., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.