Alexander DW Acholonu*
Department of Biological Sciences, Alcorn State University, Lorman, Mississippi, USA
*Corresponding Author:Alexander DW Acholonu, Department of Biological Sciences, Alcorn State University, Lorman, Mississippi, USA.
Received: July 05, 2024; Published: August 23, 2024
Citation: Alexander DW Acholonu., et al. “Review of Trichomonasis in Nigeria 1900-1997 with Report on the Prevalence of Trichomonasis at Lagos University Teaching Hospital, Lagos, Nigeria - A Retrospective Study". Acta Scientific Microbiology 7.9 (2024):26-33.
This review fulfils a need to compile and argument information on human trichomoniasis in Nigeria and highlight the public health importance of Trichomonas vaginalis. Available relevant references on this disease covering the period from 1900-1997 is provided and shows that no work was done in Nigeria on T. hominis until 1956 and on T. vaginalis until 1961. The recorded cases of T. vaginalis infection are listed and compared with those of T. hominis. There appears to be no reference to work done on T. tenax yet in Nigeria during this period. At Lagos University Teaching Hospital, 8.21% of 1304 high vaginal swabs (HVS), 1.83% of 13,898 urine samples and 0.08% of 1901 seminal fluids were positive with T. vaginalis between September 1977 and July 1979. Research on T. vaginalis in Nigeria during this period was minimal. This review fills the gap left when the earlier review was conducted. As a public health aspect of this study, epidemiology, pathogenicity, clinical manifestations, diagnosis, treatment, prophylaxis and control of T. vaginalis are discussed.
Keywords: Review; Trichomoniasis; Nigeria; 1900-1997
The three trichomonads of humans, Trichomonas tenax, T. vaginalis, and Penthatricomonas hominis, are similar enough morphologically to have been considered conspecific by many taxonomists. More recently differences between P. hominis and the other two have been recognized [1]. But their pathogenicities differ. That little attention was paid to human trichomoniasis in Nigeria during this period under review is evinced by the paucity of reports in the literature on both Trichomonas vaginalis Donne 1836 and T. hominis (Davaine, 1860) (= Pentatrichomonas hominis) and the apparent non-existence of reports on T. tenax (Muller, 1773) Dohell, 1939 (= T. buccalis). The importance of T. vaginalis, an inhabitant of the urogenital tract, as one of the most common and pathogenic etiologies of sexually transmitted diseases (STDs) of humans cannot be over emphasized. T. hominis, an inhabitant of the gastrointestinal tract, although considered to be non-pathogenic, yet it is occasionally found in considerable numbers in diarrhea stools. T. tenax which inhabits the mouth, especially in diseased gums and tartar around the teeth or in dental cavities and alveolar pus pockets is known to be non-pathogenic.
The present review was prompted by the need to augment information on the prevalence of the three human species of Trichomonas in Nigeria. It is also to fill the gap left by Asemota [2]. who reviewed Trichomonas vaginalis in Nigeria and to highlight the public health importance of T. vaginalis. While syphilis and gonorrhea are common household words known to both literate and illustrate Nigerians and bear vernacular names in the major languages of the country, the reverse is the case with trichomoniasis as a disease or infection, hence Acholonu [3]. called it a little recognized sexually transmitted disease but with grave consequences. It is also to add a few publications inadvertently omitted in Asemota’s review which covered 1998-2017.
Transmission of T. vaginalis is by coitus. However, contaminated fomites such as douche equipment, clothing and towels used in common in some families or contaminated instruments used for examination of patients are incriminated as possible means of transmission and spread especially since the organism survives from one to a few hours on dry fomites and for longer periods if moist [4]. Although according to [5], T. vaginalis may survive at the normal vaginal acidity of pH 3.8 to 4.4, infection becomes established when the acidity of the vaginal secretion is reduced.
While the transmission and spread of T. hominis is by ingestion of contaminated food, water, or hand, that of T. tenax is by a sexually related activity – kissing, and by the sharing or giving of food already in the process of mastication in the mouth as done by some, especially mothers who feed their babies by first partially masticating the solid food and then feeding it to them.
The infection causes purulent urethritis and prostate-vesiculitis in the males which may become chronic, and vaginitis associated with a characteristic profuse creamy white frothy vaginal discharge or leukorrhea in the female which may lead to excoriation or chafing of the vulva with accompanying pruritus and dermatitis of adjacent skin of the thighs. There is usually burning and itching or pruritus of the vagina. The vaginal mucosa usually becomes diffusely congested and inflamed. Frequency of urination especially nocturia, dysuria and dyspareunia are the commonest associated symptoms. Cystitis may occur. According to Mackell, and Voge [6], a possible relationship between this infection and cervical carcinoma has been suggested. While gonorrhea may be asymptomatic in females, the reverse is the case with trichomoniasis. Hence men in whom it is usually asymptomatic are known as carriers and reinfect their coital partners. Symptoms may occur when the prostate gland and seminal vesicle are infected. However, different strains of T. vaginalis differ in pathogenicity and the pathogenicity is due, at least in part, to a labile exotoxin secreted by the organism [7].
Bernfield [8] opined that trichomoniasis might be involved in infertility or conjugal sterility. The work of Sogbetun and Osoba [9] and Alausa and Osoba [10] seem to lend credence to his surmise. The former reported azoospermia in a patient harbouring numerous T. vaginalis in his seminal fluid and the latter recorded oligospermia and azoospermia in two patients respectively suffering from chronic trichomonal urethritis.
Trichomoniasis is apt to be misdiagnosed if there is a heavy reliance on clinical manifestations. This is due to the fact that there are several pathogenic micro-organisms (e.g. bacteria and yeast) of the region of the genital tract that may cause urthral, prostatic and vaginal exudates apart from T. vaginalis. Some of these are the popularly known Neisseria gonorrhoeae and Treponema pallidum, the etiologies of gonorrhea and syphilis respectively. Others are Calymmatobacterium granulomatis, Hemophilus ducreyi, Corynebacterium vaginale, Streptococcus pyognes, Staphylococcus aureus, Mycoplasma hominis, the yeast, Candida albicans as well as herpes, [11]. These should not therefore, be confused with T. vaginalis infection. Hence careful diagnosis is essential. A concomitant infection with any of these may exacerbate the symptoms and pathogenicity of trichomoniasis. Although detected at times in centrifuged or sedimented urine of men and women, vaginal and urethral discharges or secretions got from swabs or scrapings and prostatic fluid obtained by messaging the prostate gland are best diagnostic sources for the demonstration of T. vaginalis. Culture methods may be employed as necessary adjunct to increase the percentage of positive identifications and reveal or minimize false negatives of direct microscopic examination of wet film preparations.
The treatment of vaginitis caused by trichomoniasis is difficult, time consuming and not always successful. It requires patience and complete cooperation by the patient [5]. Among other things, it involves the restoration of normal vaginal epithelium and secretions, the repair of cervical lesions, the elimination of the etiological agent by the use of trichomonacides and the strict maintenance of cleanliness.
Several available chemotherapeutic agents for topical application and vaginal suppositories or inserts have been recommended for treatment such as sulfonamides and oxyquinoline derivatives. But the deficiency in those is the fact that they may fail to reach the sites of residual infection, such as glands and ducts (e.g., urinary bladder where the parasite causes cystitis). As such, oral or systemic drugs are recommended for the treatment of urogenital trichomoniasis. However, a combination or concurrent use of both produces a synergistic effect especially in resistant infections and is encouraged.
Available oral drugs have been used with some measure of success. The drugs of choice include (1) Metronidazole (Flagyl). This standard drug has significant effectiveness in the elimination of male and female trichomoniasis. With respect to side effects, furred tongue, vomiting, gastro-intestinal upset, drowsiness, headache, skin rashes, and pruritus have been reported but rarely. It requires abstinence from alcohol when used for treatment. Pregnant women tolerate metronidazole well and there is no report of any adverse effect on their offspring as stated by the manufacturer (M&B). It can be given during the first 3 months of pregnancy and during lactation if necessary. Resistance to the drug has, however, been reported from a number of areas [12]. Also it has been shown to be carcinogenic in rodents and mutagenic in bacteria and its prescription is discouraged [5]. (2) Tinidazole (Fasigyn). This is a wide spectrum of antiprotozoal drug. It is highly effective for treating male and female trichomoniasis. The side effects are said to be only mild and transitory gastro- intestinal discomforts which occur infrequently. Akinla and Ogunbi [13] reported the use of a single oral dose of 2g. of this drug in 24 patients with good results. An over-all cure rate of 100% (6 patients) was achieved in in-patients and 94% (23 of 24 patients) in out-patients at Lagos University Teaching Hospital. (3) Ornidazole (Tiberal Roche). This is a broad spectrum of antiprotozoal drug. It is remarkable for its high degree of efficiency in treating urogenital trichomoniasis in men and women and for its safety. It is well tolerated. Albeit, mild side effects such as dizziness, headache, gastro-intestinal disturbances and skin reactions occasionally occur. There is no incompatibility with alcohol as is the case with metronidazole. Although teratological and fetotoxicity studies have revealed no abnormalities, one of the contraindications is that this drug should be avoided during pregnancy except when absolutely necessary. Sandront and Labotte [14] showed through clinical and parasitological examination that a one day therapy with Tiberal Roche (1g twice on the same day) is efficaciously superior to the classic treatment with metronidazole (500 mg. daily for 10 days). It has also been shown by the manufacturers, F. Hoffmaun-La Roche & Company through investigation that a single dose therapy with 1.5 g. (3 tablets) of Tiberal Roche produces cure rates that are at least good as those achieved with a single 2g. dose of tinidazole. In short, Tiberal Roche has the following advantages: it has a high cure rate; it is well tolerated; it has no compatibility with alcohol; and it has a single dose, i.e. single dose therapy with 3 tablets only. It appears to be the most preferable drug for urogenital trichomoniasis.
These 3 drugs of choice are also effective for the treatment of trichomoniasis caused by T. hominis and T. Tenax although the two are not clinically important
Treatment is necessary in all cases of T. vaginalis infection as spontaneous cure is highly improbable. To prevent reinfection, both husband and wife need to be treated if one partner is found to be infected. This is a precondition for a permanent cure. Sexual promiscuity or extramarital sexual intercourse should be avoided after treatment of a couple. Since abstinence from sex is generally not acceptable, the best preventative method is the use of condom by men. Also males should, immediately after sexual intercourse, pass urine with high pressure or force to flush out any parasite-containing vaginal exudate that may have got into the urethral passage during coitus and in addition scrub the external genitalia thoroughly with soap and water while females should take a douche with acidic substances like lactic acid to make the vaginal pH acid and provide conditions unsuitable for T. vaginalis to survive. Use of vaginal spermicides may also be of help. Shared or common use of fomites such as underwear and towels should be avoided. Toilet seats should be cleaned thoroughly before and after use and personal hygiene strictly maintained.
A literature search conducted and covering the review period revealed the fact that apparently Cowper and Woodward [15] were the first to report on the prevalence of Trichomonas vaginalis infection in Nigeria and this is based on the work done at the University College Hospital (UCH), Ibadan on females. This means that no work was done on this parasite from 1900 to 1960. The next significant one was reported by Nnochiri [16] on a study carried out on males at Lagos University Teaching Hospital (LUTH) Lagos. A chronological list of reported cases of T. vaginalis infection in Nigeria covering the review period is provided in Table I. Reports on T. hominis in Nigeria covering the review period are also shown in Table II. It shows that apparently the first report on this species from 1900 to 1980 was made by [17] and came earlier than that of T. vaginalis. The reason for this could be the fact that while it is so easy to collect stool samples from people and examine, the collection of vaginal swabs often meets with repulsion or frown and considered a social taboo or something unthinkable to do at the time. As stated above, the literature appears to be devoid of reports on T. tenax. The two tables reveal the following: (1) that although still relatively minimal, the work done on T. vaginalis (13 with present contribution included) is more than that on T. hominis (8 recorded). (2) that much of the work is done on both this far has been in and around the University Teaching University, Ibadan and Lagos University Teaching Hospital, Lagos. (3) that it is imperative that follow-up studies of this kind be done if found lacking.
An exhaustive search was made for relevant publications on trichomoniasis in Nigeria covering the review period. It is hoped that anyone(s) inadvertently omitted will be included by subsequent investigators.
The prevalence study on trichomoniasis conducted at Lagos University Teaching Hospital is based on the microscopic examination of 1304 high vaginal swabs (HVS) and 1901 seminal fluids from adults (21 years and above) in-patients and out-patients as well as 13899 centrifuged urine samples obtained also from adult in-patients and out-patients of both sexes between the months of September 1977 and July, 1979. 107 (8.21%) of the swabs, 152 (0.8%) of the seminal fluids and 116 (1.83%) of the urine samples were positive with T. vaginalis. 104 (1.30%) of 8,014 female urines and only 12 (0.20%) of 6,484 male ones were positive.
The prevalence of T. vaginalis in swabbed females is lower than that very first one (35.5% of 90 swabs) recorded by Cowper and Woodward (1961) at UCH. but more than the latest (6.9% of 578) recorded by Sogbetum., et al. (1977) also at UCH. But in males, with their urine samples examined, the frequency of infection (0.20% of 6,484) is a minutia when compared with the 7.89% of 152 males reported by Nnochiri (1968) to have suffered from urethritis caused by T. vaginalis. This study shows that T. vaginalis is more prevalent in women (1.30% of 8,014 female urine infected) than in men in Lagos and that male infections have abated considerably since Nnochiri’s report (1968) conducted in the same locality as the present one. But this result should be taken with some reservation as the people involved were not a selected group but rather those with cases of clinical urethritis, vaginitis or pruritus submitted for diagnosis by hospital doctors from various departments (e.g. Medicine, Obstetrics and Gynecology, out-patients Department, etc.). A randomly selected group of villagers or students will give a better insight to the degree of prevalence of Trichomoniasis vaginalis in the area.
The significance of this study, therefore, is more than anything else, the evidence hereby given that trichomoniasis is not uncommon in Lagos and for that matter in Nigeria, and the portrayal of the fact that research on Trichomoniasis vaginalis in Nigeria is seemingly minimal and mainly centered around one locality – University College Hospital, Ibadan, now called University of Ibadan, Oyo.
The percentage of infections recorded here are, obviously, less than the actual prevalence. This opinion is buttressed by the fact hat in Nigeria people very much practice self-medication. Many people covertly go to Pharmacists, Private, or Native Doctors (Herbalists) instead of hospitals for treatment when they contract any malady that is sexually related. They go to the hospital only when all efforts to effect a cure fail.
The Nigerian Civil War of 1967-1970 brought in its wake some moral decadence. Industrialization or “Modernization” fanned or aggravated the situation. The country was then and now flooded with imported pornographic materials. Sequel to the increased sexual promiscuity in the country, is a continued and increased prevalence of Trichomoniasis vaginalis and other sexually transmitted diseases(STDs). The control of this disease is and should be recognized as a public health problem along with gonorrhea and syphilis. In anticipation of ever increasing prevalence of sexually transmitted diseases, clinics for STDs should be set up in various parts of the country for diagnosis and therapy. Treatment should be free or within the reach of everyone needing it.
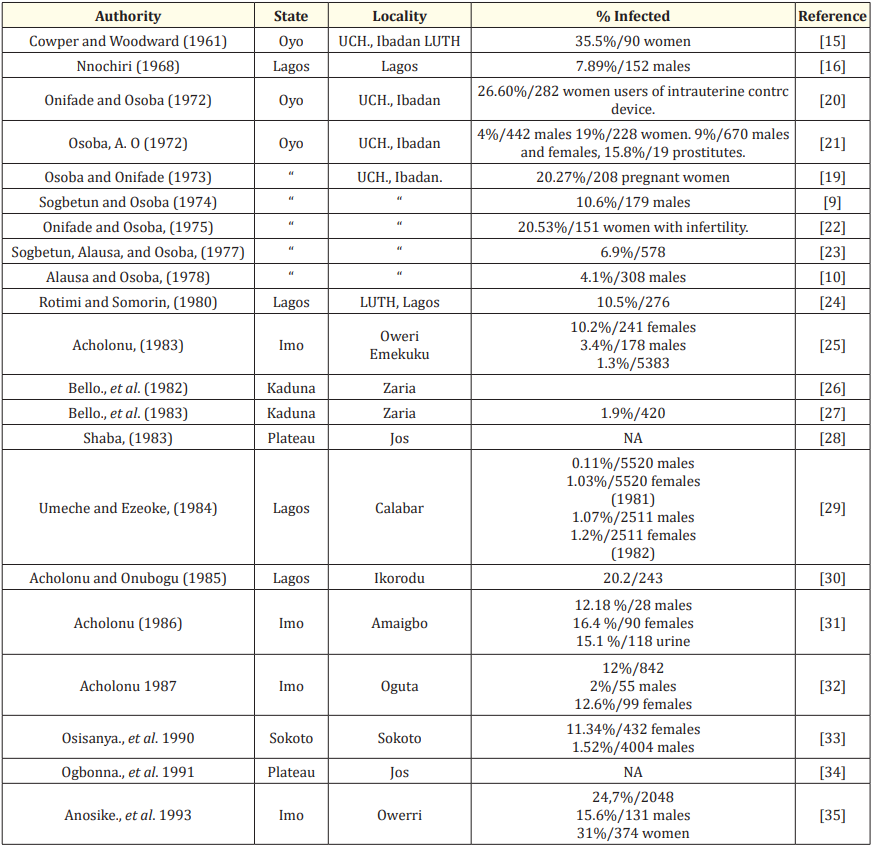
Table 1: Recorded Cases of Trichomonas vaginalis infection in Nigeria (1900-1997).
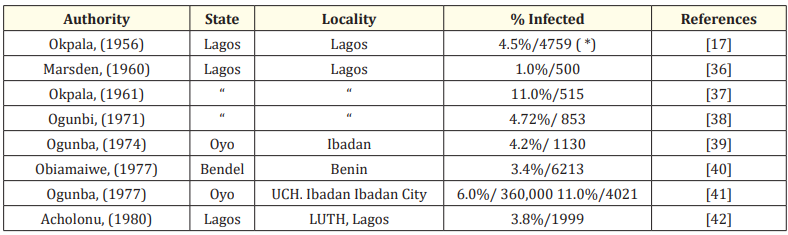
Table 2: Recorded Cases of Trichomonas homninis infection in Nigeria (1900-1997).
(*)Reported as flagellates and includes T. hominis, Girdia intestinalis and Chilomastix mesnili.
The need for conducting a laboratory test before treating for trichomoniasis and other sexually transmitted diseases cannot be over emphasized as this alone permits the determination of the exact etiological agent. Reliance on and treatment based on impromptu clinical or symptomatic diagnosis of patients should be discouraged. The consequences of misdiagnosis could be far reaching. While penicillin can be used to treat gonorrhea and syphilis, it cannot for trichomoniasis as T. vaginalis is resistant to it. So a misdiagnosis of trichomoniasis for gonorrhea will leave trichomoniasis unperturbed or the treatment ineffective. The finding by Oveinnikov., et al. [18] that trichomonads are capable of phagocytosing gonococci and thus may serve as a reservoir of gonococcal infection and actuate its resurgence in cases of mixed infection should be given serious consideration in Nigeria where mixed infection of the two is prevalent as reported by Osoba and Onifade [19]. A concurrent treatment for both is advisable. It is strongly recommended that some research be carried out on T. tenax to know among other things, whether it is prevalent in Nigeria.
I wish to acknowledge the technical assistance of Jean Louis Cyuma Cyubahiro, a graduate student in the School of Agriculture at Alcorn State University, Mississippi, USA.
Copyright: © 2024 Alexander DW Acholonu., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.