Jorge Eduardo Méndez Sánchez1, Noé Zaragoza Arias2*, Juan Carlos Orozco Oregon3, José Sebastian Villalón López3, José Antonio Villegas Velasquez3 and Marianela Centeno Flores3
1Principal Investigator, First Year Resident of the Specialization Course in Oncological Surgery, IMSS-UMAE T-1, Colonia Los Paraísos, León, Guanajuato
2Principal Investigator, Specialist in General Surgery, Physician Attached to the IMSS General Surgery Service-UMAE T-1, Colonia Los Paraísos, León, Guanajuato
3Associate Researcher, Specialist in Oncological Surgery, Physician Attached to the IMSS-UMAE T-1 Oncological Surgery, Colonia Los Paraísos, León, Guanajuato
*Corresponding Author: Noé Zaragoza Arias, Principal Investigator, Specialist in General Surgery, Physician Attached to the IMSS General Surgery Service-UMAE T-1, Colonia Los Paraísos, León, Guanajuato.
Received: September 09, 2024; Published: October 23, 2024
Citation: Noé Zaragoza Arias., et al. “Prognostic Factors in Patients with Phyllodes Tumor of the Breast in the High Specialty Medical Unit. National Medical Center in Mexico"". Acta Scientific Gastrointestinal Disorders 7.11 (2024):47-51
Background: Phyllodes tumors of the breast are a rare fibroepithelial neoplasm that accounts for less than 1% of all breast malignancies. (3) The incidence of Phyllodes tumors is low, 0.3%-0.9% of all breast tumors.
Objective: To identify prognostic factors in patients with Phyllodes tumor of the breast in the High Specialty Medical Unit. National Medical Center in Mexico
Material and Methods: The diagnostic study was a prospective, descriptive, observational study, and a comprehensive document was prepared on the prognostic factors in patients with Phyllodes tumor of the breast.
Demographic data, margins according to the histology, tumor size, and surgical treatment were recorded
Results: The general findings were: the average age was 29 years old, female sex corresponded to 100%, male sex to 0%. According to the size variable, after its statistical analysis the result was 1.5 cm representing 41.66% of the total sample.
Wide resection was administered in 10 patients (83.34%), simple mastectomy in 1 patient (8.33%) and modified radical mastectomy in only 1 patient (8.33%).
Conclusion: In conclusion, we report the experience and findings at our center. The phyllodes tumor in our population is less than 5 cm in size, which is reflected in a lower number of mastectomies and a higher number of wide resections, in contrast to other reports or other centers where the tendency is for large tumors that are mostly taken to mastectomies.
Keywords:Breast Tumor; Phyllodes Tumor; Prognostic Factors
Phyllodes tumors of the breast are a rare fibroepithelial neoplasm that accounts for less than 1% of all breast malignancies [3]. The incidence of Phyllodes tumors is low, 0.3%-0.9% of all breast tumors [3]. Phyllodes is derived from the Latin Phyllodium, meaning "leaf-like," based on a gross pathologic description of a leafy, bulky, cystic breast tumor [3].
In 1982, the World Health Organization (WHO) histologically classified Phyllodes tumors as benign, borderline, and malignant based on their histopathologic features, which has been widely accepted [3].
Benign tumors are more frequent, constituting between 35% and 64%, borderline tumors between 7% and 40% of cases, while malignant tumors reach up to 30%. They have unpredictable behavior regardless of their histological grade.
Local recurrences and distal metastases rarely occur in benign Phyllodes tumors, while they are common in borderline and malignant Phyllodes tumors [3].
Due to limited data, the etiology of Phyllodes tumors is unknown and risk factors are not yet clearly identified; however, Latina women and East Asians who were born in Central or South America and live in the United States are at increased risk [4].
Phyllodes tumors occur almost exclusively in women; however, a few cases have been reported in men, all of which were associated with gynecomastia [4,5]. The median age of presentation in Phyllodes tumors is 45 years, with the age ranging from 9 to 93 years and Asians being diagnosed at a significantly younger age than other groups [6].
Phyllodes tumors usually present clinically as a benign breast mass, sometimes with rapid growth [7-10].
A benign Phyllodes tumor is characterized by well-defined tumor margins, mild stromal cellularity, absent or mild atypia, < 5 mitotic figures per 10 high-power fields, and absence of stromal overgrowth or malignant heterologous components [11-15]. A borderline Phyllodes tumor is characterized by typically well-defined or focally penetrating tumor margins, absent or focal stromal overgrowth, moderate stromal cellularity, mild or moderate stromal atypia, and absence of malignant heterologous components (16-18). Mitotic activity is in the range of 5-9 per 10 HPF. A malignant Phyllodes tumor characterized by marked stromal cellularity and atypia, permeative margins, stromal overgrowth, and mitotic activity of at least 10/10 HPF [19,20].
Surgery is the main treatment for Phyllodes tumors of the breast. However, due to its unclear clinical presentation, pathological behavior and difficult preoperative diagnosis, there still seems to be a problem in management [21].
The extent of surgery remains debatable because the surgical resection margin is thought to be associated with local recurrence. In addition, numerous clinical studies recommend wide tumor excision with a 1 cm clear margin which may cause great difficulty in achieving good aesthetic results [22]. However, recent studies show that there is no direct relationship between the local recurrence rate and the width of negative margins.
The objective of this study was to determine the prognostic factors of Phyllodes tumors of the breast, to provide appropriate treatment for each type of tumor found and avoid further local recurrences, surgical reinterventions and improve overall survival.
The diagnostic study was a prospective, descriptive, observational study. A comprehensive document was prepared about the prognostic factors in patients with Phyllodes tumor of the breast at the “High Specialty Medical Unit. Specialty Hospital No. 1. National Medical Center of Bajío”, in the city of León, Guanajuato, Mexico. No experimental action was performed during the study.
Start Date: January 2023 to August 2024.
Using non-probabilistic sampling, a total of 12 patients were included during the research period.
The study was approved by the ethics and research committee of the electronic registry system of the Health Research Coordination of the Mexican Social Security Institute, Leon, Guanajuato, Mexico (Registry R-2024-1001-022, March 20, 2024). Demographic data, margins, tumor size and surgical treatment were recorded.
Statistical analysis was performed using IBM SPSS software and Excel program Descriptive statistics were used to determine the distribution of the variables. The Quantitative Variables were applied the Saphiro Wilks normality test, observing a free distribution so they are reported as median and range. Categorical variables are reported as frequencies and percentages.
A total of 12 patients were identified. All patients were females. The average age was 29 years old. According to the size variable, after statistical analysis the result was 1.5 cm, representing 41.66% of the total sample.
Histopathological variants were 9 benign, (75%), 3 borderline (25%), and 0 malignant tumors (0%). Surgical treatment according to histology as well are presented in table 6, the importance is offering the best treatment according to the size of the tumor and avoid suboptimal treatment.
Wide resection was administered in 10 patients (83.34%), simple mastectomy in 1 patient (8.33%) and modified radical mastectomy in only 1 patient (8.33%).
In our study we observed that in most patients a wide resection was offered in order to achieve negative margins, no malignant phyllodes tumors of the breast were identified, however, in 2 patients who were classified as borderline, 2 types of surgical option were offered, both simple mastectomy and modified radical mastectomy.
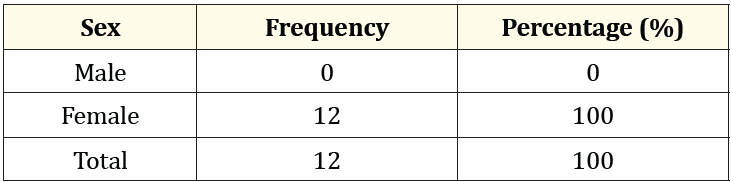
Table 1: Gender percentage in patients with Phyllodes tumor of the breast
A total of 12 women were observed, representing 100%, since during the study and based on the sample analyzed, no Phyllodes tumor of the breast was identified in any man.
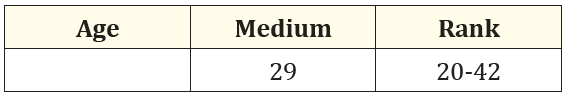
Table 2: Medium age of patients with Phyllodes tumor of the breast.
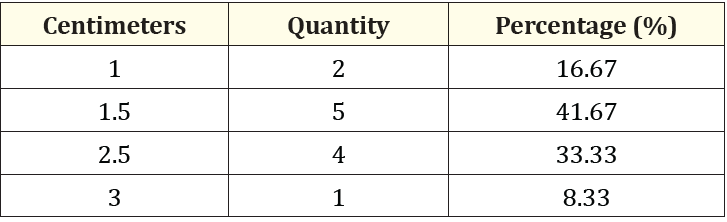
Table 3: Percentage of size in patients with Phyllodes tumor of the breast.
According to the results of our study, a higher percentage of tumor size of 1.5 cm was observed, representing 41.66% of the total sample analyzed.
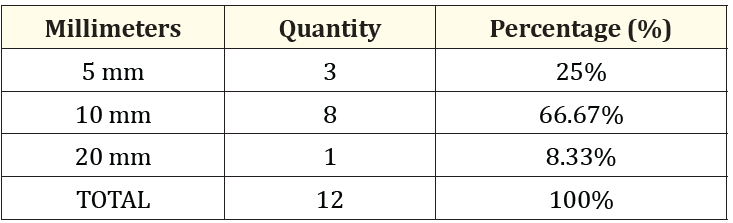
Table 4: Percentage of margins reported in patients with Phyllodes tumor of the breast.
For benign phyllodes tumors, we aim for a clear margin but do not require a wide margin. Negative margins are acceptable.
We observed that the margins are an important parameter in the recurrence of all types of tumors. In our study, specifically in Phyllodes tumors, they are part of one of the prognostic factors for recurrence. Therefore, in the graph shown, we observe that the majority had an adequate margin since most of them were benign.
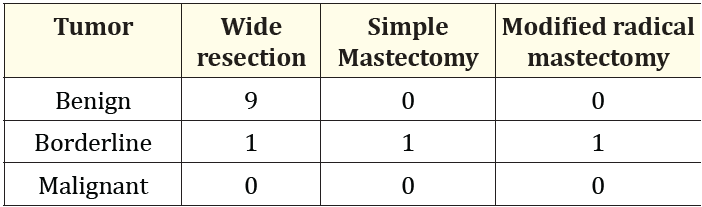
Table 5: Surgical Treatment by histological subtype in patients with phyllodes tumor of the breast.
It was observed in our study that most patients had wide resection, since the histology was mostly benign phyllodes tumor, only 1 patient was offered modified radical surgery due to the borderline component, no malignant tumor was found in our sample.
Discussion
According to the literature published by Cheng., et al. the median age of presentation of Phyllodes tumors is 45 years, with an age ranging from 9 to 93 years, and Asians are diagnosed at a significantly younger age than other groups. In our study, a much younger median of patients was found, represented at 29 years, which does not lead us to think that breast tumors are increasingly found in younger patients.
Most phyllodes tumors of the breast are fast-growing tumors of considerable size, which on average can vary from 5 mm to 40 cm; according to what was reported in our sample, the largest tumor identified was 3 cm.
Regarding the frequencies of histopathological variants, benign phyllodes tumors are reported from 50 to 72.3%, borderline tumors in 16.2 to 35%, and malignant tumors in 11.4 to 24.3% of cases.
In our study we observed that 9 were benign (75%), 3 borderline (25%) and no malignant tumor was identified.
According to several authors such as Bernstein, the average size of benign tumors is 4 cm, borderline 5 to 6 cm and malignant tumors larger than 6 cm. In our study, we did not observe this trend since the smallest tumor identified was 1 cm and the largest was 3 cm, and according to what has been reported in the literature, tumors equal to or larger than 3 cm suggest a malignant process, however in our population this pattern was not identified.
Surgery is the main treatment for Phyllodes tumors of the breast. However, due to their unclear clinical presentation, pathological behavior and difficult preoperative diagnosis, there still seems to be a problem in their treatment plans [21].
In the past, simple mastectomy was the recommended treatment for borderline and malignant tumors [21].
Breast-conserving surgery was safe and adequate even for malignant Phyllodes tumors if complete excisions were achieved.
It is reported that 69.8---90.2% of phyllodes tumors are treated with wide resection alone and 9.8---30.1% with mastectomy.
In our institution wide resection was performed in 10 patients (83.34%), and only one simple mastectomy (8.33%) and one modified radical mastectomy were performed (8.33%).
Due to what is reported in the literature, mastectomy is proposed in tumors larger than 3 cm, however in our sample we found tumors from 1 cm, which is why wide resection was mostly performed.
For benign variants, tumor-free margins of 1 mm have been accepted or even in some reports negative ink margins are accepted, for borderline and malignant histologies a margin of 1 -2 cm is recommended.
We obtained 91.67% margins equal to or less than 1 cm and 8.33% greater than 1 cm.
Conclusion
In conclusion, we report the experience and findings at our center. The phyllodes tumor in our population is less than 5 cm in size, which is reflected in a lower number of mastectomies and a higher number of wide resections, in contrast to other reports or other centers where the tendency is for large tumors that are mostly taken to mastectomies.
Ethical Aspects
This research protocol complies with the ethical standards set out in the Nuremberg Code, the Declaration of Helsinki and its 2013 amendment, as well as the bioethical principles set out in the Belmont Report. Also conforms to those established in nom-012-SSA3-2012, which establishes the criteria for the execution of research projects for health in human beings. The study was submitted for review by the Local Health Research Committee and the Research Ethics Committee of the hospital unit and approved with the institutional registration (R-2024-1001-022, March 20, 2024).
Copyright: © 2024 Noé Zaragoza Arias., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.