Zener JosePaez Milano*, Sofia Anais Montilla Soto, Ramo ́n Alirio Vergara Hernandez, Arianny Estefaní ́a Santiago Santiago, Fabiana Carolina Camino Perdomo and Marí ́a Claudia Bracho Arellano
Coloproctologist Unit, Laparoscopic and General Surgery Department, Hospital Universitario de los Andes, School of Medicine, Université de Los Andes, Me'rida Venezuela
*Corresponding Author: Zener JosePaez Milano, Coloproctologist Unit, Laparoscopic and General Surgery Department, Hospital Universitario de los Andes, School of Medicine, Université de Los Andes, Me'rida Venezuela.
Received: September 02, 2024; Published: October 03, 2024
Citation: Zener JosePaez Milano., et al. “Early Local Complications of Intestinal Ostomies". Acta Scientific Gastrointestinal Disorders 7.11 (2024):04-14.
Introduction: In gastrointestinal surgery, due to multiple causes, it is frequent to perform procedures that require derivation or abocation of the gastrointestinal tract to the surface in order to feed the patient (gastrostomies, jejunostomy) or to eliminate waste products (ileostomies and colostomies), however, many of these patients tend to become complicated, and they not only have to live with the stoma but also have to worry about the complications derived from its confection.
Objective: To determine the frequency of early local complications of intestinal ostomies.
Methodology: retrospective descriptive observational retrospective longitudinal study with the purpose of evaluating the early local complications that appear in patients who had ostomies confectioned in the General Surgery Service of the Instituto Autonomo Hospital Universitario de los Andes during the period between January 2015 and June 2021. We reviewed 254 medical records of patients who underwent this procedure, of which 81 patients had early complications, 2 corresponded to jejunostomies, 20 to ileostomies and 59 corresponded to colostomy.
Results: The age group in which the complications occurred was between 40-49 years; in relation to the segment of intestine that was abducted to the abdominal wall, 66.7% were terminal and 33.3% in loop or lateral; the segment of intestine with the highest percentage of externalization (48.1%) was the descending colon; The most frequent cause that led to the creation of the ostomy was intestinal obstruction with 39.5%; the complications presented by the patients showed that edema was the main complication with 67.9%, partial disinsertion in 39.5%, dermatitis in 38.3%, defascation in 28.4%, abscesses in 25.9% and malpositioning in 23.5%.
Conclusion: More than half of the patients do not undergo successive evaluations in the outpatient clinic, so that in the future they may relapse in complications that may be preventable, besides not restoring those patients who have a temporary stoma
Keywords: Complications; Ostomy; Colon; Jejunum; Ileum; Colostomy
In the history of ostomies, Praxagoras of Cos was the first to perform enterocutaneous fistulas to treat intestinal obstruction, which were performed by percutaneous puncture with hot iron. The first successful stoma was performed by Duret (1793) by performing a colostomy on a 3-year-old child with an imperforate anus. In 1952, Brooke revolutionized the history of stomas by recommending mucosal eversion, a principle that is still used today [1].
The term "ostomy" comes from the Greek "stoma" (stoma) which means "mouth", it is a surgically created opening between a hollow viscera and the abdominal wall, which has the purpose of supplying food to the patient (gastrostomies and jejunostomies) or eliminating waste products (ileostomies and colostomies), these can be temporary or definitive [2,3].
The creation of an intestinal stoma is part of the surgical management of pathologies that affect the gastrointestinal tract, such as inflammatory diseases and neoplasms, such procedure is not risk- free and predisposes patients to various complications [4]. Globally, it can be considered that at least half of the patients will experience at least one stoma-related complication during their lifetime. However, there are studies that describe up to 70-80% with one or more complications or even upto 96% after 3 weeks post-surgery [5,6].
Early complications are those that occur in the immediate postoperative period (up to 30 days) and represent 39-82% of all complications [5-7]. However, there are isolated studies in hospitals of the capital region where they report that the percentage of early complications is around 45% [5]. Among the early complications we have: skin irritation, ischemia, necrosis, retraction and collapse, stenosis (obstruction), hemorrhage, infection with suture dehiscence [1,7].
Stoma complications have been related to multiple risk factors, including emergency surgery, inflammatory bowel disease, age, obesity, as well as those directly related to the technique used andthe characteristics of the stoma (height and shape).8 These early complications can have a significant impact on patients' recovery and quality of life, which is why understanding these complications is essential for healthcare professionals, as it allows for early detection and appropriate management. In addition, the optimized patient must adapt to a new lifestyle, which involves learning the care, handling and manipulation of waste collection devices, as well as developing the ability to identify possible complications.
The objective of this study is to determine the frequency of early local complications in patients with intestinal ostomies who have been treated at the General Surgery Service of the Instituto Autonomy Hospital Universitario de los Andes. In addition, to determine if there is a relationship between risk factors, the surgeon's experience and the appearance of complications presented by these patients once the procedure has been performed.
A retrospective descriptive observational retrospective longitudinal study was carried out in order to evaluate the early local complications that appear in patients who underwent ostomies in the General Surgery Service of the Instituto autonomous Hospital Universitario de los Andes during the period from January 2015 to June 2021. A total of 254 clinical histories of patients who underwent this procedure were reviewed, of which 81 patients had early complications, 2 corresponded to jejunostomies, 20 to ileostomies and 59 corresponded to colostomies. Inclusion criteria were patients over 16 years of age of both sexes, operated by the General Surgery Service at the Instituto autonomous Hospital Universitario de los Andes, who underwent jejunostomies, ileostomies or colostomies, with successive controls at least 30 days after the stoma was performed. Patients operated on in other health centers and who underwent ileostomy or colostomy during the procedure, patients operated on by the pediatric surgery service and patients who died in the immediate postoperative period due to causes other than the pathology studied were excluded.
Descriptive statistics are presented in frequency distribution tables, with absolute and relative numbers, for qualitative variables and in measures of central tendency and dispersion for quantitative variables.
During the research, the sample of patients was standardized and identified with a number, for its stratification and anonymity; likewise, it was approved by the Ethics Committee of the institution.
For the statistical analysis, the IBM SPSS professional program, version 22 for Windows, was used with the information collected in the Excel data for subsequent processing in which, in turn, basic statistical processes such as descriptive tables and graphs including proportions or percentages for qualitative variables were used. Measures of central tendency (mean, median and mode) and measures of dispersion (rances, variance, standard deviation) to analyze quantitative variables and determine the statistical significance of p < 00.05.
During the period under study, 254 patients underwent ostomy surgery at the General Surgery Department of the Hospital Universitario de los Andes, 81 of them presented complications in the first 30 days after surgery and met the criteria to be part of the present study.
It could be seen that the age group where the complications occurred was between 40 - 49 years, with 27.2%, followed by 50 - 59 years with 24.7%, 60 - 69 years with 21.0%, being the groups with less percentage those of 30 - 39 years and those under 30 years, with an average age of 53.47 ± 16.21 years with a minimum age of 18 years and a maximum of 96 years; with respect to gender it could be seen that the female sex predominated with 51.9% over the male with 48.1% (figure 1).
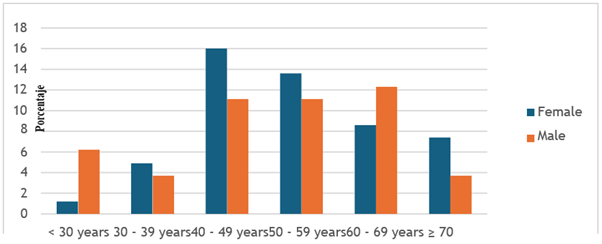
Figure 1: Age Group ánd Gender. Pátients with intestinál Ostomy ánd complicátion. Generál Surgery Service. IAHULA. Jánuáry 2015 - June 2021.
On the other hand, when we investigated the background and comorbidities of the patients who underwent surgery, it was found that 53.1% suffered from arterial hypertension, 50.6% from obesity, 31.1% from diabetes and 23.5% from underweight; it should be noted that 54.3% of the patients had a smoking habit (Figure 2).
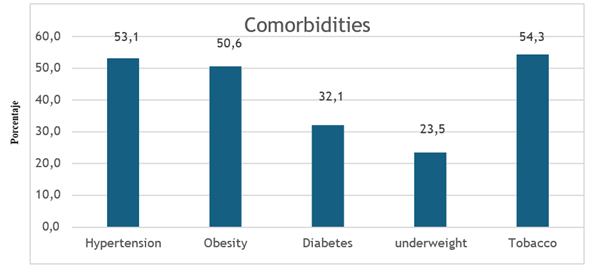
Figure 2: Comorbidities ánd Psychobiologicál Hábits of Pátients who underwent Intestinál Ostomy ánd presented complicátions. Generál Surgery Service. IAHULA. Jánuáry 2015 - June 2021.
Regarding the type of intestinal ostomy, it was observed that 93.8% were performed for temporary purposes and 6.2% were permanent or definitive, in relation to the segment of intestine that was placed in the abdominal wall, 66.7% were terminal and 33.3% in loop or lateral, these data are shown in figure 3,4.
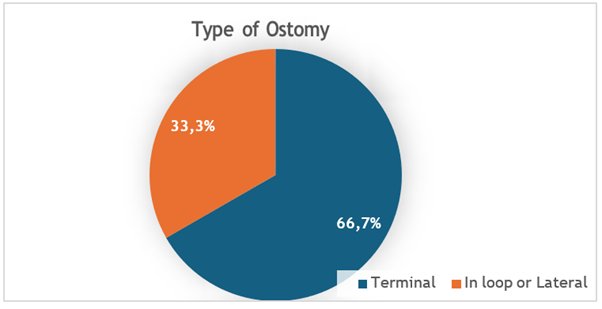
Figure 3: Type of Ostomy performed in the Generál Surgery Service. IAHULA. Jánuáry 2015 - June 2021.
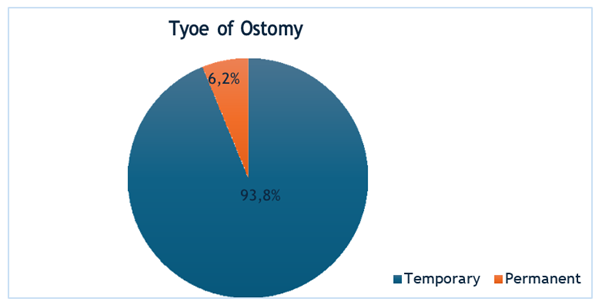
Figure 4: Type of Ostomy performed in the Generál Surgery Service. IAHULA. Jánuáry 2015 - June 2022.
It was also found that 48.1% of the bowel segment exteriorized was descending colon, 24.1% ileum, 23.5% transverse colon, with the jejunum and right colon being the segments that were exteriorized the least, as shown in table 1.
However, upon inquiring about the etiology that led to the creation of the ostomy, it became evidente that the main reason was intestinal obstruction (39.5%), anastomosis leakage (34.6%), ovarian cancer (22.2%), colon cancer (19.8%), and trauma (17.3%), and shown in table 2.
When investigating the time elapsed between the performance of the intestinal stoma and the appearance of complications, it was found that 48.1% of the patients presented complications between 1 and 7 days, 30.9% in the first 24 hours and 21.0% between 8 and 30 days, as shown in table 3.
In relation to the complications presented by the patients, edema was the main complication (67.9%), partisan disinsertion (39.5%), dermatitis (38.3%), defasciation (28.4%), abscesses (25.9%). The number of cases (23.5%). figure 5.
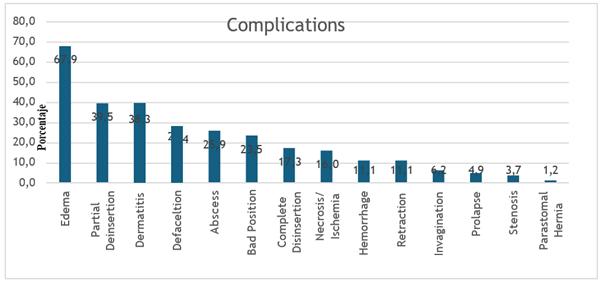
Figure 5: Complicátions presented by intestinál Ostomy. Generál Surgery Service. IAHULA. Jánuáry 2015 - June 2021.
Source: Dátá taken from Clinicál Histories. Department of Heálth Records ánd Státistics IAHULA. 2021.
When the cause of intestinal ostomy was related to the year of residency of the person who performed it, it was observed that 48.8% of intestinal obstructions were performed by a second-year resident, 25.0% by a third-year resident and 21.9% by a first-year resident, with no statistical significance; With regard to anastomotic leakage, it was found that 42.9% of the ostomies were performed by a third year resident, 21.4% by a second and fourth year resident respectively, not being statistically significant; with regard to ovarian cancer, 50.0% of the ostomies were performed by a second year resident, 27.8% by a third year resident and 22.2% by a first year resident, as shown in figure 6.

Figure 6: Relátionship of the cáuse with the yeár of the resident who performed the intestinál Ostomy. Generá Surgery Service. IAHULA. 2015 - June 2021.
Source: Dátá taken from Clinicál Histories. Department of Heálth Records ánd Státistics IAHULA. 2021.
When the complications were related to the year of residence of the person who performed the intestinal ostomy, it became evident that 34.5% of the patients who presented edema corresponded to second year residents and 32.7% to third year residents; of those who presented partial disinsertion, 46.9% corresponded to second year residents and 34.4% to third year residents; of those who presented dermatitis, 48.4% of the ostomies were performed by a second year resident and 35.5% by a third year resident, as well as defascation, 39.1% by a second year resident and 26.1% by a first and third year resident, with no statistical significance, as shown in table 4.
After relating the complications to the segment of bowel exteriorized, it was found that of those who presented edema, 50.0% were descending colon; of those who presented partial disinsertion, 40.6% were descending colon and 31.3% ileum, with no statistical significance; in those who presented complete disinsertion, 35.7% were descending colon with p = 0.006, retraction with 55.6% in descending colon with p = 0.009 and prolapse with 80.0% in transverse colon with p = 0.047 being statistically significant, as can be seen in table 5.
When relating the complications with the type of intestinal ostomy, it was found that 60% of the patients who presented edema were terminal, 40% lateral or loop, 62.5% of those who presented partial disinsertion were terminal and 37.5% lateral or loop, 92.3% of the patients who presented necrosis/ischemia were terminal and 7.7% lateral or loop, finding statistical significance p = 0.028; it should be noted that terminal ostomies were the ones that presented more complications, clearly exemplified in table 6.
Now, in relation to the complication and the time in appearing it was observed that those who developed edema 65.5% was between 1 - 7 days, 29.1% less than 24 hours, as for partial disinsertion 81.3% was between 1 - 7 days and 15.6% between 8 - 30 days, of those who presented dermatitis 64.5% between 1-7 days and 29.0% between 8 - 30 days, of those who presented defascation 65.2% was between 1-7 days and 26.1% less than 24 hours, malposition was between 1-7 days and 38.1% between 8 - 30 days, malposition was between 1-7 days and 29.0% between 8 - 30 days, of those who presented abscesses 61.9% was between 1-7 days and 38.1% between 8 - 30 days,Those who developed abscesses 61.9% between 1-7 days and 38.1% between 8-30 days, malposition was 52.6%, it should be noted that statistical significance was found in almost all the complications with the time of appearance except in complete disinsertion, retraction, invagination and in the parastomal hernia, exemplified in table 7.
Likewise, in relation to the complications and previous marking, 72.7% of the patients who presented edema were not marked and 27.3% were marked, of those who presented disinsertion 71.9% were not marked and 28.1% were marked, of those who presented dermatitis 71.0% were unmarked, of those who presented defascation 78.3% were unmarked, of those who presented abscess 90.5% were unmarked, being statistically significant, and of those who presented abscess 90.5% were unmarked, being statistically significant,Of those who presented dermatitis, 71.0% were without marking, of those who presented defascation 78.3% had no previous marking, of those who presented abscess 90.5% had no marking, being statistically significant as well as malposition with p = 0.021 and p = 0.007 respectively, these results are expressed in table 8.
Finally, it was found that the restitution of intestinal transit of patients with stomas was only performed in 19.8% of which 50.0% were performed between 4 to 6 months, 25.0% between 7 to 9 months, 18.8% between 9 to 12 months and 6.3% more than 12 months (Table 9).
An intestinal ostomy is a surgically constructed digestive opening to the intestinal wall, depending on the intestinal segment exteriorized, it derives its name, in order to enable the communication of the internal part of the intestinal tract with the external part, where the elimination of feces and urine occurs [9,10]. A colostomy is a connection between the colon and the skin of the abdominal wall, likewise the ileostomy comprises the exteriorization of the ileum to the abdominal skin [10].
Complications in this type of procedure are present and the rates vary widely in the literature, from 23.5% to 67.5% [11], in addition to representing high costs in the public health system, longer hospital stay and therefore a decrease in the patient's quality of life; therefore, early diagnosis and management of this type of situation is of vital importance.
In the General Surgery Service of the Hospital Universitario de los Andes, the complications derived from these procedures were analyzed during the period from 2015 to June 2021, epidemiological characteristics, cause and clinical condition of the patient were analyzed in order to carry out the stoma confection and the local complications that appeared during the first 30 days. Similarities and differences were obtained with respect to research by different authors.
The total population studied consisted of 81 patients, higher than that used by Reyes Hernandez (2018) where he analyzed postoperative complications in ostomized patients, [12] but lower tan the population studied by Stegensek., et al. (2016) who analyzed 143 records of ostomized patients in their work of urinary and fecal fecal diversions in a specialized center [13].
The average age of the group of patients studied was 53.47 with standard deviation of 16.21, the age ranges ranged from 18 to 94 years, this result is similar to that found by Reyes Hernandez in 2018 whose average age was 52.39 years [12].
Regarding the results of comorbidities, psychobiological habits and other associated factors, it was shown that the predominant pathology in these patients was arterial hypertension with 53.1%, followed by obesity with 50.6%, diabetes with 31.1%, underweight/malnutrition with 23.5% and more than half of these patients presented smoking habits 54.3%, This data is relevant because obesity plays a fundamental role in the appearance of complications, the excess of adipose panniculus either in the abdominal wall or in the mesos makes difficult the surgical technique, the fixation of the ostomy mouth to the wall, bringing as a consequence that at the end an ostomy with tension is obtained causing the appearance of complications, this last item of risk factors was compared with the study of Ruiz., et al. [8]. who related the TCS thickness and stoma complications, since the BMI does not reflect the lean mass of a patient nor does it distinguish between visceral or peripheral obesity; however, no statistically significant p was obtained between the TCS thickness and said complications, contrary to Ruiz., et al. In this regard, it is mentioned that the outflow of more liquid stool can damage the integrity of the skin at various levels. Other research, similar to this study, showed that obesity was related to a higher frequency of peristomal complications [15].
With respect to the study of diabetes as a risk factor, there is discordance in the literature. Authors such as Persson., et al. do not associate diabetes as a risk factor, as is the case in our study; however, Arumugam does obtain statistically significant results that associate diabetes with a higher percentage of complications [18].
Likewise, the main reason for ostomy was intestinal obstruction with 39.5%, as well as Reyes Hernandez (2018) who showed that the main cause was non-tumor obstructive acute abdomen with 33.96% and tumor obstructive acute abdomen (neoplastic) with 26.42% [12].
Among the early complications, edema was the most frequent with 67.9%, but ostomies performed in terminal segments of the gastrointestinal tract are the most common, being the most common necrosis/ischemia with 92.3%, having a statistical significance in terminal ostomies (p = 0.028), these data disagree with Reyes Hernandez (2018) who presented as complication edema in 45% of his series and periostomal dermatitis in 30.19% of the cases [12].
Regarding the time of onset of complications, it is evident that most of them occur during days 1 and 7 after the procedure, finding statistical significance, perhaps due to the inexperience of the patients to handle it, in addition to the lack of trained personnel to guide them in the first weeks of the surgical act. These data differ from Jayarajah (2016) who in his case series describes that complications generally occur in the following 2 weeks after the procedure, but they agree that terminal colostomies are the ones that present greater complications [16].
Finally, it was found that only 19.8% of all patients underwent intestinal restitution, a low percentage in comparison with other data reported in the literature that report between 60-65% restitution in these patients.
Ostomies are procedures frequently performed during emergency surgery. According to this study, patients with special conditions such as previous diseases, obesity, underweight and tobacco use are the main candidates for complications.
Edema is the most important complication, followed by partial or complete disinsertion and dermatitis, which is why it is vitally important that the physicians working on the ward know how to identify them and provide timely treatment, in addition to orienting family members and patients in the management of the stoma at home.
More than half of the patients do not undergo successive evaluations in the outpatient clinic, so that in the future they may relapse in complications that may be preventable, in addition to not restoring those patients who have a temporary stoma.
Own funds.
None to declare.
Copyright: © 2024 Zener JosePaez Milano., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.