Robson Uwagoya1* and Marcus Cezillo2
1Member of Grupo de Pesquisa e Extensão em Cirurgia (GPEC), São Paulo/SP, Brasil
2General Chief of Grupo de Pesquisa e Extensão em Cirurgia (GPEC), São Paulo/SP, Brasil
*Corresponding Author: Robson Uwagoya, Member of Grupo de Pesquisa e Extensão em Cirurgia (GPEC), São Paulo/SP, Brasil.
Received: May 23, 2024; Published: September 16, 2024
Citation: Robson Uwagoya and Marcus Cezillo. “Hepatic Trauma: The Evolution of Management". Acta Scientific Gastrointestinal Disorders 7.10 (2024):13-15.
Hepatic trauma is one of the most common abdominal injuries in patients with severe trauma [1]. The anterior location within the abdominal cavity and the fragile parenchyma, covered by the easily ruptured Glisson's capsule, render this organ vulnerable to injury [2].
The diagnosis and treatment of hepatic trauma have significantly evolved with the use of modern diagnostic and therapeutic tools [3-5]. Up until two to three decades ago, most cases of abdominal trauma with possible injuries to parenchymal organs were treated with exploratory laparotomy [6]. During this period, various innovative multimodal approaches gained traction, such as the endovascular management of bleeding, which greatly increased the possibility of non-operative management (NOM) in selected patients.
Minimally invasive approaches (MIAs), such as videolaparoscopy, have also gained prominence and indication in the initial treatment phase, as an extension of NOM, in cases of late surgical indication or diagnostic uncertainty in hemodynamically stable patients with blunt trauma and, more recently, also in penetrating injuries [7,8].
Despite advancements in the diagnosis and treatment of hepatic trauma, exploratory laparotomy has maintained its fundamental role in severe hepatic trauma with unstable patients, especially in settings lacking the material and human resources to support NOM and MIAs. This decision-making process has evolved over the years by utilizing trauma severity classifications that categorize patients with specific anatomical hepatic injuries. Accordingly, major trauma associations have proposed classifications such as those by the AAST - The American Association for the Surgery of Trauma (table 1) and the WSES - World Society of Emergency Surgery (Table 2), aiming to formulate guidelines for the optimal treatment of this injury.
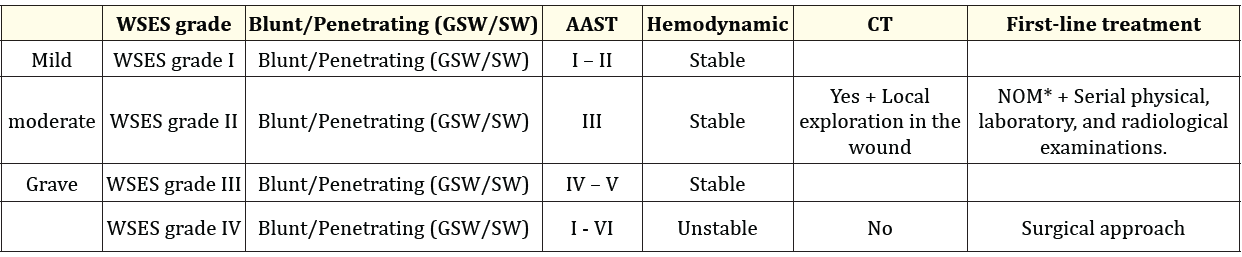
Table 1: SW (Stab Wound), GSW (Gunshot Wound); *NOM should only be recommended in centers capable of precise diagnosis of the severity of hepatic injuries and trained in intensive management (clinical observation and hemodynamic monitoring in a high-dependency/intensive care environment, including serial clinical examination and laboratory testing, with immediate access to diagnostics, interventional radiology, and surgery, as well as immediate access to blood and blood products; **Exploration of wounds near the lower costal margin should be avoided, except in strictly necessary cases, due to the high risk of intercostal vessel injury).
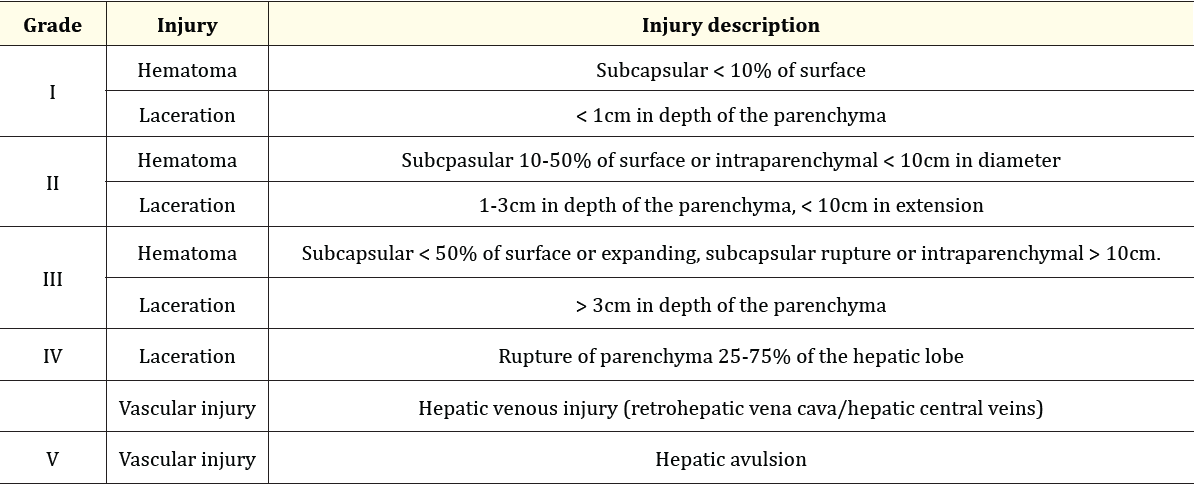
Table 2: Classification of hepatic injury by The American Association for the Surgery of Trauma (AAST).
Patientselection capabilityis closely related to the accuracy of available methods [9]. Inaddition to hemodynamic stability and absence of injuries requiring immediate surgery, imaging examination, more precisely computed tomography (CT), is necessary for treatment definition. This concept applies to both penetrating and blunt trauma mechanisms, with attention to the energy involved [10,11].
Currently, even borderline or transient responders, without other indications for laparotomy, may be considered for NOM in trauma centers. This advanced strategy requires a multidisciplinary approach to deal with the complexity of moderate and severe hepatic injury. When determining the ideal treatment strategy, the anatomical description of hepatic injuries is fundamental but not sufficient. The decision whether patients need to be operated on or undergo NOM is primarily based on hemodynamic status, associated injuries, and the anatomical degree of hepatic injury [12]. Continuous monitoring and intensive care are preferable during follow-up of patients undergoing NOM. In addition, serial physical and laboratory examination are indispensable, and often radiological examination may also be necessary to exclude late rebleeding or associated injury [13].
With the classification of injuries and the possibility of patient grouping, careful selection has allowed forsaferindicationof MIAs inparenchymal organ traumas, especiallyinhepatic trauma. Laparoscopy has gained ground and become the first choice in cases of delayed surgery and diagnostic doubt, presenting benefits for clinically stable patients, especially in obese and pediatric patients [14,15]. Still within the minimally invasive modality, angioembolization has allowed for broader reach of endovascular treatment in trauma. Indications may range from initial operative hemostasis in a stable patient or compensated patients with hepatic trauma showing arterial blush (active contrast extravasation on CT) [16]. Another application is its use as an adjunctive hemostatic tool in patients suspected of uncontrolled arterial bleeding, despite emergency laparotomy and attempted hemostasis [11,17]. Recent evidence suggests that post-emergency surgery hepatic angiography indication reduces mortality in grade IV/V hepatic injuries [18].
Non-complex biliary tract injuries resulting from trauma can be managed endoscopically. However, more complex injuries require exploratory laparotomy (EL). Not only this type of injury, but alsocases of hepatic traumawithunstable patients requiringimmediate surgery, such as in damage control surgery or even liver injury repair in stable patients in trauma centers lacking resources for MIAs or when there is no surgeon and team qualified to indicate this therapeutic modality [13,19,20].
Copyright: © 2024 Robson Uwagoya and Marcus Cezillo. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.