Mohd Adilin Yaacob*, Raden Shamilah Radin Hisam, Nurhainis Ogu Salim, and Noor azian MD Yusuf
Parasitology Unit, Infectious Disease Research Centre, Institute for Medical Research, Block C3 & C7, Level 2, National Institutes of Health (NIH), Ministry of Health Malaysia, No. 1 Jalan Setia Murni U13/52, Seksyen U13, Bandar Setia Alam, 40170 Shah Alam, Selangor; Malaysia
*Corresponding Author: Mohd Adilin Yaacob, Parasitology Unit, Infectious Disease Research Centre, Institute for Medical Research, Block C3 & C7, Level 2, National Institutes of Health (NIH), Ministry of Health Malaysia, No. 1 Jalan Setia Murni U13/52, Seksyen U13, Bandar Setia Alam, 40170 Shah Alam, Selangor; Malaysia.
Received: August 06, 2024; Published: August 15, 2024
Citation: Mohd Adilin Bin Yaacob., et al. “A 6-Years Retrospective Study of Suspected Amoebiasis in the Institute for Medical Research, Malaysia". Acta Scientific Gastrointestinal Disorders 7.9 (2024):09-13.
This retrospective study was undertaken to evaluate Entamoeba histolytica infections in suspected cases of amoebiasis for six years (2014-2019) from diagnostic samples received at the Parasitology Unit, IMR. A total of 1248 serum samples were involved, comprising subjects from 0 to 90 years old with a mean age of 48.7 ± 18.8 years old. From the analysis, 28.5% (356/1248) were seropositive for anti-E. histolytica IgG antibody. Of these, 32.7% (310/947) of seropositivity was due to an amoebic liver abscess (ALA), and 15.3% (46/301) of positive cases were related to other symptoms. More males (34.3%) acquired anti-E. histolytica antibody than a female (15.2%) with a ratio of 2:1 and showed a statistical significance (p < 0.0001). Infection was more predominant in the adult age group from 18-40 years old than in another age group. There was a significant association with the presence of amoeba antibodies concerning the ethnicity of the patient with 25.4% of positive cases being from Malay ethnic (p < 0.05) followed by other ethnicities (p < 0.0001), respectively. This study highlights that amoebiasis infections are not uncommon in Malaysia and require a proper management and intervention strategy to reduce the burden of the disease in the community.
Keywords: Amoebiasis; Odd Ratio; Entamoeba Histolytica; ELISA; Amoebic Liver Abscess
Amoebiasis is a clinical disease caused by Entamoeba histolytica, a protozoan parasite from the family of Entamoebidae. Worldwide, it has been estimated that up to 50 million people are affected by E. histolytica, primarily in developing countries, and it is responsible for over 100,000 deaths a year [1]. Most infections are asymptomatic, which may start with ingesting the mature cyst in contaminated food or water, followed by transformation to motile trophozoites in the small intestine and then the large intestine [2]. Afterward, the invasive intestinal disease may manifest in several weeks with complaints of cramping, abdominal pain, watery or bloody diarrhea, and weight loss [3]. Disseminated extraintestinal manifestations such as liver abscess, pneumonia, purulent pericarditis, and cerebral amoebiasis were also reported. E. histolytica is unique among amoeba because of its ability to disrupt the intestinal mucosa, causing intestinal disease, amoebic colitis, and the capacity for hematogenous spread, resulting in potentially fatal abscesses and extraintestinal diseases [3,4].
In Malaysia, waterborne protozoan disease like amoebiasis is closely related to sanitation system and personal hygiene practices, particularly in aboriginal settlements (Orang Asli) and rural areas. Orang Asli is the indigenous minority of West Malaysia, while native people are indigenous people from multi ethnicities in East Malaysia. Varied prevalence of E.histolytica/E.dispar/E.moshkvskii has been reported in such areas. For example, E.histolytica/E.dispar infection prevalence among Orang Asli tribes living in Perak, Pahang, and Negeri Sembilan recorded a prevalence ranging from 1% to 61% [5-9].
Diagnosis of amoebiasis infections in many countries relies commonly on microscopic examination of stool samples for the presence or absence of E. histolytica. Liver abscess is the most common manifestation of extraintestinal amoebiasis [10]. ELISA is the most popular technique used to investigate the epidemiology of symptomatic amoebiasis due to its reliability and ease of performance [11]. Furthermore, serodiagnosis can detect infection (present and past) in a broader timeline because IgG antibody titer does not drop dramatically after recovery [12]. In Malaysia, most studies focus on the prevalence of amoebiasis in aboriginal groups [6,8,13], but the prevalence among hospitalized patients is generally underreported. The present study reviews the seroprevalence of amoebiasis attributed to E. histolytica in Malaysia and possible risk groups and common clinical presentations for the disease.
Data collection and analysis.
Archived data of amoeba serology analysed using ELISA kit DRG® Entamoeba histolytica IgG (DRG International Inc., NJ, USA) from 2014 to 2019 were retrieved. Hospitalized patients (1248 samples) with traceable biodata and complete clinical symptom history were selected. The respective socio-demographic information such as gender, age, and ethnicity were retrieved from pathological forms. Ethnicity was grouped into five categories: Malay, Chinese, Indian, Other ethnics (Orang Asli and Native people), and non-Malaysian. Data were tabulated and analysed using Microsoft Excel 2016 and IBM SPSS version 20 (SPSS Inc., Chicago, IL, USA). Bar and line graphs were employed to illustrate the trend of amoebiasis over the years. The percentage described the studied population's characteristics, including seropositivity according to gender, age, ethnicity, and clinical presentation. The Odds Ratio (OR) and 95% confidence interval (CI) were determined based on univariate analysis to identify the potential association factors with the presence of E. histolytica infection. P value <0.05 was considered statistically significant.
As shown in figure 1, the annual seropositivity of amoebiasis gradually increased from 24.6% in 2014 to 35.2% in 2018 and declined in 2019 (23.6%). The average seropositivity rate for 6 years of analysis was 28.5% (356/1248). Concerning gender, male samples recorded a significantly higher seropositivity rate (34.3%, p < 0.0001) compared to their female counterparts (15.2%) as depicted in table 1. Besides, the seropositivity rate varied in different age groups, ranging from 38.6% among 18-40 years of age to 8.3% among subjects 7-12 years old. In terms of ethnicity, other ethnics were the most significantly affected with a seropositivity rate of 56.3% (P < 0.0001) followed by Malay (25.4%, P < 0.005). The top five reported clinical presentations in seropositive cases were liver abscesses (32.7%), followed by cholangitis, other abscesses, jaundice, and sepsis. About a quarter (86/356) of positive cases recorded were from East Malaysia and three-quarters (270/356) were from West Malaysia.
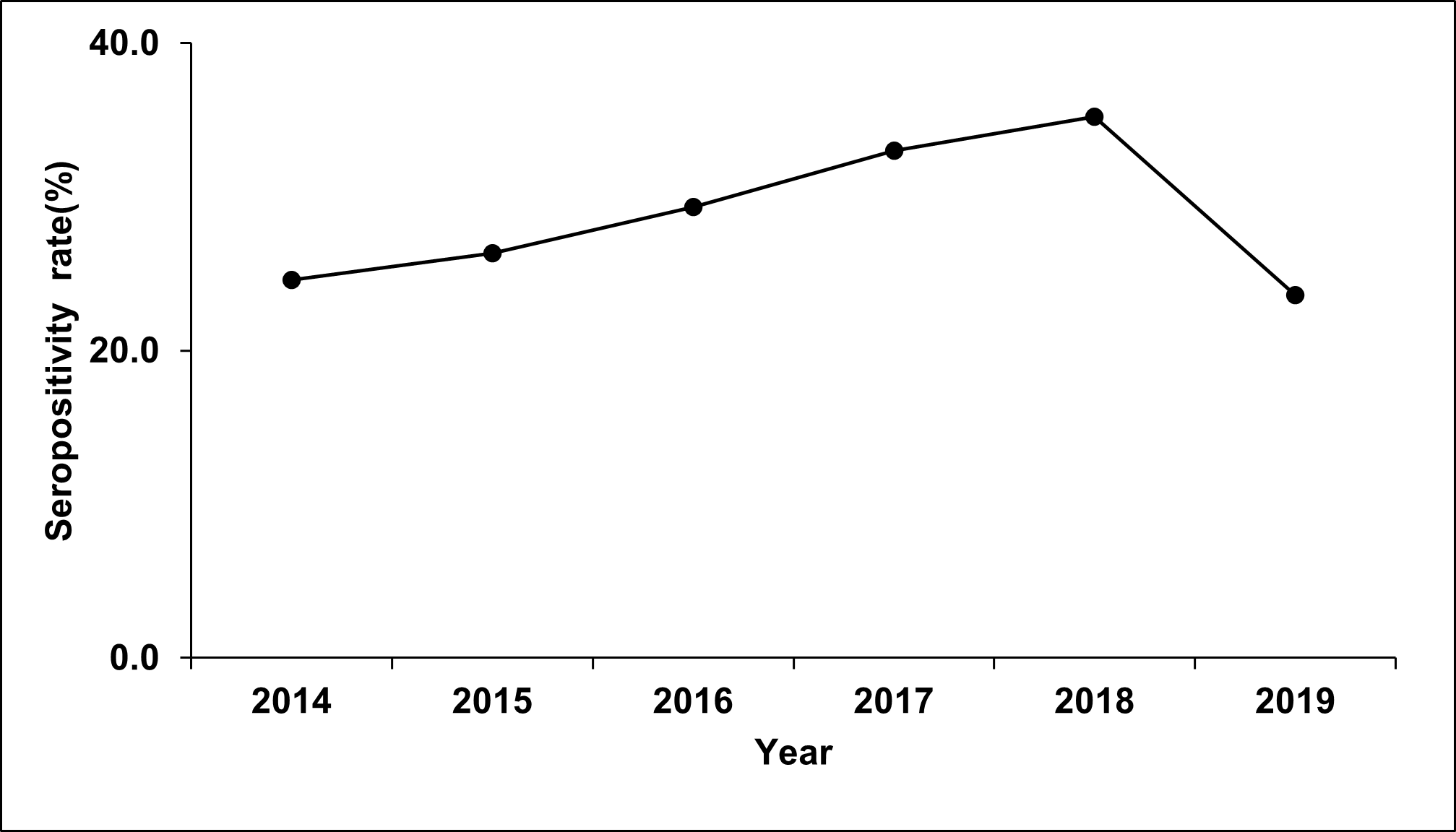
Figure 1: Annual amoeba seropositivity rate from suspected amoebiasis patients investigated by IMR from 2014 to 2019.
Although various authors have reported the prevalence of intestinal amoebiasis in selected communities, seroprevalence on extraintestinal amoebiasis in the Malaysian community from hospitalized cases is rarely reported. Globally it was estimated that the incidence rate due to liver abscess at 2.3 cases per 100000 people, but substantially higher rates had been reported in Taiwan (17.6 cases per 100000) [17-19]. Other clinical features associated with seropositive, such as fever, diarrhea, abdominal pain, eosinophilia, jaundice, and sepsis, could be symptoms/signs related to ALA or intestinal amoebiasis. However, medical and travel history in these cases was incomplete and could not contribute to a definite clinical diagnosis. Suspected clinical cases for extraintestinal amoebiasis can best be confirmed by serology, sonographic, or radiology procedure followed by prompt treatment.
As shown in table 1, analysis regarding gender and ethnicity, males are frequently more affected than females. The result agreed with other published findings, which reported that invasive amoebiasis infected more men than women, with a ratio ranging from 3:1 to 12:1 [16]. This disparity is unknown, but such observation may be due to oestrogen stimulating effect on the phagocytic system leading to a better humoral and cellular response against E. histolytica infection among women [18,19].
Surprisingly, while amoebiasis in infants rarely happens, 30.5% (11/36) of the studied cases were reported, requiring further investigation, particularly on risk factors contributing to such cases. The highest seropositivity rates are observed among adults aged 18-40, followed by 41-60. It is unclear why older adults were more prone to ALA. However, inadequate sanitation, the impact of daily lifestyle, working conditions, and lower host immune response may contribute to this vulnerability [20,21]. It is also possible that the extraintestinal amoebiasis acquired could be due to prolonged bouts of amoebic diarrhoea that go unnoticed because the diarrheal episodes tend to appear and disappear without treatment. Over time, inflammation of the bowel lining promotes leakage and creates routes of dissemination of trophozoites into adjacent areas and via the bloodstream to multiple organs.
Regarding geographical area, West Malaysia regions seem to have a higher rate of acquiring amoebiasis with OR (0.6195-0.3441, <0.0001) than East Malaysia. This may be due to the location of the IMR institute in the West region of Malaysia. Sample bias may contribute to the higher cases of amoebiasis reported in the West rather than the East region. Malaysia has a multiracial population that represents Malays (about 50%), followed by Chinese (22.4%), and Indians (6.8%). Therefore, the highest number of seropositive among Malays could be due to a sample bias. The high prevalence of ALA also is not due to any ethnic predisposition. However, it reflects the overall socio-economic status, level of environmental sanitation, hygiene practice, and other socio-cultural practices pertaining to diets and eating habits [9,22-24]. In contrast, a study conducted by Jamaiah in 1999 showed that 45% of ALA were seen in Chinese, followed by Indian 35%. In addition, Malays formed the predominant group affected by amoebic dysentery forming 40% of the cases, followed by Chinese [22].
Non-Malaysian may have acquired infections while staying in our country or acting as carriers. This group comprises travellers or migrant workers from neighbouring countries such as Myanmar, Bangladesh, Philippines, Indonesia, Nepal, Vietnam, and Thailand, endemic for amoebiasis (data not shown) [25]. Hence, there is a high chance that the patients acquired infections in their hometown before being diagnosed positive. Nevertheless, as the patient's travel history is not included in the pathological forms, it limits our understanding to asses and elaborates more on this statement. Imported cases of amoebiasis from endemic countries by foreign workers or travellers are concerning, given the lack of a monitoring system for parasitic infection, particularly on our border. Therefore, it will be interesting to conduct antibody screening among visitors and foreign workers of the potential risk of transmission, i.e., in food processing industries, restaurants, and food stalls, and constantly remind them to maintain good personal and food preparation hygiene.
Study Limitation
While most of the studies conducted in Malaysia are limited to focus groups or certain ethnics and only bound to specific places such as Orang Asli communities which live in substandard environments, this present study, on the other hand, gives more information on the actual burden of infections among generalized communities that been hospitalized due to E. histolytica infections. These patients with different backgrounds and ethnicities give a broader perspective on the actual burdens of infections on the Malaysian community. Nevertheless, we acknowledged that this study utilized the existing seroprevalence result from diagnostic samples. Moreover, the socio-demographic and risk factors analysis were based on the pathological forms in which bias might be introduced. Besides, this study also has missing data on important risk factors such as sexual practices and entire travel history. In addition, the seroprevalence test does not distinguish the present infection from the past infections.
The present findings highlighted that E. histolytica infections remain prevalent in Malaysia. ALA is the most common clinical presentation associated with amoebiasis, and ELISA is the most suitable technique to diagnose extraintestinal amoebiasis, especially for ALA clinical presentation. Due to limitations on the disease burden, the study is helpful to improve our understanding of the disease's actual burden and helpful in planning for amoebiasis management in our country. As no vaccine is available to prevent amoebiasis, the preventive measures on food and water safety and health promotion on hygiene and lifestyle are essential aspects that must be considered. Furthermore, household contacts of patients with amoebiasis should be screened as amoebiasis may spread among family and household members.
Copyright: © 2024 Mohd Adilin Bin Yaacob., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.