J Kittu1*, V Aditi2, Pramila M3, Geetha S4
1 Reader, Department of Public Health Dentistry, Rungta College of Dental Sciences and Research, Bhilai, Chhattisgarh, India
2 Assistant Professor, Department of Public Health Dentistry, Faculty of Dentistry, Jamia Millia Islamia, New-Delhi, India
3 Professor, Department of Public Health Dentistry, MR Ambedkar Dental College and Hospital, Bangalore, Karnataka, India
4 Senior Lecturer, Department of Public Health Dentistry, MR Ambedkar Dental College and Hospital, Bangalore, Karnataka, India
*Corresponding Author: Kittu Jain, Reader, Department of Public Health Dentistry, Rungta College of Dental Sciences and Research, Bhilai, Chhattisgarh, India.
Received: March 11, 2019; Published: March 21, 2019
Citation: J Kittu., et al. “Measuring the Impact of Oral Health Related Quality of Life from Womb till Post-Partum”. Acta Scientific Dental Sciences 3.4 (2019): 75-82.
Introduction: Pregnancy is characterized by complex physiological changes due to hormonal change. These changes can have adverse affect on oral health. Also these oral disorders can have a significant impact on physical, social & mental well-being during pregnancy and thus, on their quality of life.
Aim: To assess the oral health status and oral health related quality of life during pregnancy and 3 months post-partum among the women attending hospital in Bangalore city.
Methods: The study consisted of 80 pregnant and 80 non pregnant women. Oral health status was assessed using Plaque index (PLI), gingival index (GI), Decayed Missing Filled teeth index (DMFT). Oral health related quality of life (OHRQoL) was assessed using Oral Health Impact Profile-14 (OHIP-14). After collecting baseline data, follow up was done at three monthly intervals for three times in both the groups.
Results: The results showed that the study group had significantly higher PLI score in the post partum and a significantly higher GI score in the second trimester of pregnancy, when compared with the non-pregnant women. There was no significant difference in the overall OHIP-14 scores between the two groups although pregnant women showed significantly higher score for functional limitation in the first trimester and for the physical pain and psychological discomfort in the second trimester when assessed longitudinally during pregnancy and three months post partum.
Conclusion: The results of the study showed more gingival changes and poorer OHRQoL during second trimester of pregnancy.
Keywords: Oral Health Status; Oral Health Related Quality of Life; Pregnancy; India
PLI: Plaque Index; GI: Gingival Index; DMFT: Decayed Missing Filled Teeth Index; OHRQoL: Oral Health Related Quality of Life; OHIP-14: Oral Health Impact Profile-14.
Pregnancy is a unique moment in a woman’s life, and is characterized by complex physiological changes with the most significant “Hormonal change”. These changes in hormones can have adverse affect on oral health along with the general health [1]. The expectant mother may be involved in a multitude of extra activities, which can lead to a neglect of her own oral care and can have impact not only on the woman but also on the developing foetus [2].
Research has suggested that the pregnancy hormones act as growth factors by satisfying the naphthoquinone requirement for the oral gram negative anaerobes during pregnancy resulting in a multitude of oral diseases [3]. The high levels of progesterone during pregnancy can cause an imbalance that may enhance the growth of the oral bacteria resulting in pregnancy gingivitis occurring in 30 to 100% of all pregnant women [2]. A woman’s immune system may also be off killer during pregnancy and this may cause a greater susceptibility to gingivitis-causing bacteria [3]. Although there is little evidence that pregnancy increases the risk of dental caries, some studies have suggested that changes in the oral environment during this period may predispose to an increased incidence of dental caries [4]. Regarding the oral lesions, pyogenic granuloma (or pregnancy tumor) seems to be common in pregnant women, with a prevalence of about 5% in the gestating female population [5].
Apart from the burden of oral diseases, there is also a growing acceptance of the fact it can pose a significant impact on physical, social and mental well-being of an expectant female and thus, on her Quality of life (QoL) [6]. The Oral Health Impact Profile (OHIP -14) is a well-known method for identifying dimensions in OHRQoL. It measures people’s perceptions of the social impact of oral disorders on their well-being [7].
In particular, to the authors' knowledge, limited work has assessed the impact of OHRQoL among pregnant women for exploring the impact of certain factors, such as pain, on the OHRQoL or the factors that affect OHRQoL but no long term evaluation impact has been done so far [6,8,9]. Hence, the present study is undertaken to assess the changes in oral health status and OHRQoL during three trimesters of pregnancy and 3 months postpartum amongst the women attending hospitals in Bangalore city, Karnataka, India.
A longitudinal Case Control study was conducted amongst pregnant women reporting for antenatal checkup in the two hospitals of Bangalore City in Karnataka State, India. A sample of 60 pregnant women satisfying inclusion and exclusion criteria in two randomly selected government hospitals formed the study (case) group. The control group was also selected from the two government working women hostels matched for age, socio economic status and oral hygiene practices. Both the Case and Control group were selected randomly by a lottery method for the purpose of this study.
Inclusion criteria: women experiencing first pregnancy (case group); women who have not been pregnant previously (control group). Exclusion Criteria: women with the habit of tobacco chewing or smoking, having systemic conditions such as diabetes, leukemia, hormonal disorders, using contraceptive pills, having menstruation period (control group). Voluntary written informed consent was obtained from both the groups.
Ethical approval was obtained from the Institutional Review Board of M.R Ambedkar Dental College and Hospital, Bengaluru (MRADC&H/ECIRB/29/12-13) prior to the commencement of the study. This study was conducted in accordance with the Declaration of Helsinki.
The sample size was estimated based on prevalence of gingivitis in pregnancy (92%) taken from earlier study [2] employing the statistical formula, n= zα2pqD/L2, where α-error was set at 5%. Design effect (D) was taken 2 for convenience sampling. Sample size obtained was 67, increased to 20% to compensate for the loss to follow up in anticipation of longitudinal study. Thus the final sample size of 80 subjects was reached for both the groups.
A pre-structured proforma in English constituting three parts was employed for the purpose of the study. Part one consisted of informed consent and socio-demographic information such as name, age, socio-economic status (Kuppuswamy’s scale, 2012) [10] and oral hygiene practices. Phone number and complete address were also recorded to further follow up the subjects and future correspondence. Second part included the evaluation of the impact of oral health in pregnancy via complete oral health examination with the help of Plaque index (PLI), Gingival index (GI), Decayed Missing Filled Teeth WHO criteria 1997 (DMFT). Third part consisted of the evaluation of the impact of oral health in pregnancy on quality of life using Oral Health Impact Profile-14 (OHIP-14), as a measurement of OHRQoL [7]. The OHIP-14 questions were translated from English to Kannada (local language) for convenience and feasibility of the study and then translated back to English to ensure the meaning of question remains the same. Suitability of the questionnaire was checked by inviting six experts to provide comments. As the questionnaire seemed to be appropriate for evaluation of the study objectives, no revisions were made. Cronbach's alpha was found to be 0.71, indicating acceptable reliability.
The study was scheduled to last for a 12-month period from November 2013 to November 2014. The investigator underwent formal training for clinical examination by the expert for 1 week before the commencement of the study. The intra and interexaminer reliability was then checked and came out to be Kappa value as 0.83 suggesting acceptable agreement. The subjects were made to sit on the chair comfortably with the examiner standing beside. The type III clinical examination as recommended by American dental Association was followed throughout the study. The subjects were instructed to fill only the socio-demographic data, oral hygiene practices and OHIP-14 questionnaire. They were asked to approach the investigator, in case of any doubt regarding filling of the proforma for clarification.
The clinical examination was then carried out by the investigator under adequate natural light and the Plaque index (PLI), Gingival index (GI), Decayed Missing Filled Teeth WHO criteria 1997 (DMFT) were recorded for both the groups.The baseline clinical examination and filling of OHIP -14 questionnaire proforma was carried out at the first visit for both the groups. The follow up for the study and control groups was then done for three times at three monthly intervals which were corresponding to the end of the second trimester, third trimester, and three months post-partum for the study group.
The outcome variables in each group were described using a simple descriptive measure of mean and standard deviation. The dependent variables were checked for normality of distribution using Kolmogrov-Skirov test using Statistical Package for the Social Sciences Version 18.0 (IBM Corp., Armonk, NY, USA), data was found to be normally distributed (p>0.05. The outcome measures were compared between the groups using Student’s t test for comparison of the mean scores of PLI, GI, CPI, DMFT and OHIP14 between the groups. Repeated Measures Analysis of Variance (RMANOVA) was used to assess the changes in the mean scores of PLI, GI, DMFT and OHIP-14 within the study group during their subsequent visits.
The study was started with the 80 subjects in the study group as well as in the control group. Thirteen subjects dropped out in the three follow ups in study group (drop out rate – 16.25%) and 10 subjects dropped out in control group (dropout rate - 12.5%). Analysis was done only for the subjects who were present in all the follow ups. Mean age in the study group was 24.29 + 3.42 years and 24.63 + 3.35 years in control group. Out of total subjects, majorities (80%) belonged to lower class and lower middle class in both study and control group. All the subjects in both the groups brushed their teeth with tooth brush and tooth paste. Majority of them in both the group (study - 65%; control - 62 %) brushed once daily and rest of the subjects brushed twice daily.
Comparison of oral health status between the two groups is shown in Table 1. Mean PLI score was significantly different (p = 0.02) in the post partum period, whereas mean GI score was significantly different (p = 0.003) in the second trimester and no significant difference in the DMFT score in all the four examinations.
Table 1: Comparison of Mean Plaque Index score, Gingival Index score and DMFT score among case and control group.
† Student t-test; *p< 0.05 significant
Although there was an increase in the mean plaque score from the first trimester to 3 months post partum, but the difference was not significant (p = 0.64). For the mean GI score, there was an increase from first to second trimester, followed by continue drop till post partum period. Repeated measures ANOVA revealed a significant difference (p = 0.17) in the scores of the four examination and post hoc analysis found that difference was significant (p = 0.025) between the second trimester and 3 months post partum. There was no significant difference (p = 0.76) found as the scores of the DMFT remained constant throughout the study from first trimester to post partum (Figure 1).
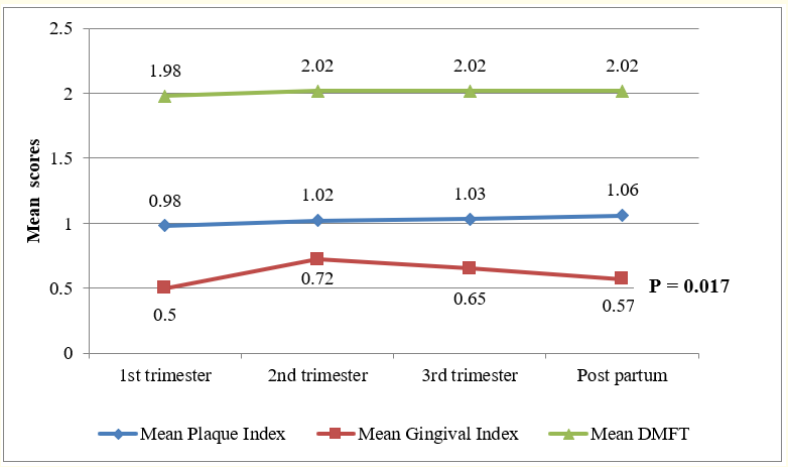
Figure 1: Mean score changes for PLI, GI, DMFT during pregnancy and post partum.
The comparison of the mean OHIP-14 scores for each question between the two groups revealed a statistically significant difference for three questions out of fourteen, with study group having higher mean scores than the control group. The difference was found in the first and the second trimester, but not in the third trimester and post partum as shown in Table 2. A statistically significant difference was found only between three dimensions out of the seven, with study group having higher mean scores than the control group while the comparison in overall mean OHIP-14 scores between the two groups came out to be insignificant Table 3.
Table 2: Comparison of scores for each question of OHIP – 14 among study group and control group.
*p < 0.05 significant † Student’s t test
Table 3: Comparison of scores for each dimension of OHIP – 14 and overall score among study group and control group.
† Student’s t test
There was a significant change in the mean score of OHIP-14 dimensions, functional limitation (p = 0.001) and psychological discomfort (p = 0.023), whereas in the rest of the five dimensions there was insignificant change. Post hoc analysis showed that the mean score for functional limitation in the first trimester was significantly higher than the scores in the next three follow ups. For the psychological discomfort dimension, mean scores was significantly high in the second and third trimester (Figure 2).
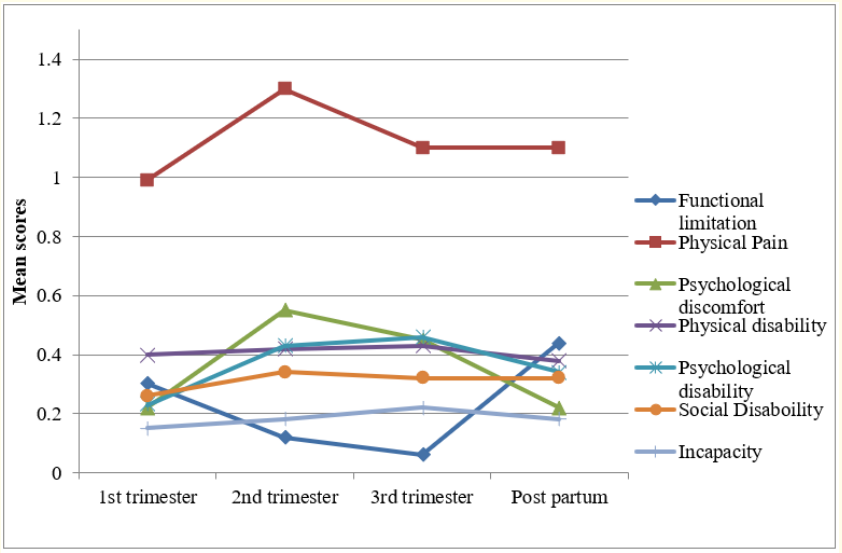
Figure 2: Mean score changes for OHIP-14 dimensions during pregnancy and post partum.
To the author’s knowledge, it is first of its kind for evaluating the long term impact of pregnancy on oral health related quality of life from pre-term till post-partum period. This design was employed for establishing the true temporality between hormonal changes during pregnancy and post-partum period. Being a longitudinal study, the lost to follow-up was already taken into due consideration prior to the commencement of the study. The overall dropout rate was 16.25% and the probable reasons for drop-out were: change in their consulting doctor/miscarriage/change of contact details/ went to parent’s place for delivery. While similar rate of attrition was in the control group (change of hostel/city). Hence the subjects left in study group and control group were 67 and 70 respectively, which satisfied the sample size estimated previously.
The subjects in both the groups belonged to the lower strata as majority of the females visiting the government hospitals in India belonged to that strata only and were from the peri-urban/ rural communities of the Bangalore city, Karnataka, India. This was verified by Kuppuswamy’s scale as it is an appropriate scale for evaluating the socio-economic status of the urban and peri-urban communities [10]. Age, oral hygiene practices and socio-economic status of both the groups were well matched as these variables can act as confounders.
The present study inclusion and exclusion criteria’s were specifically considered based on the knowledge of previous literature search like the previous pregnancies were excluded as it could have left a major impact on oral health, similar to the study done by Tilakaratne., et al. [3] in contrast with the previous studies [11,12] which did not excluded this variable. The subjects were excluded who were using oral contraceptive pills or having their menstruation period. Fluctuation in estrogen/progesterone has been noticed in these conditions which may affect the periodontal health [13,14]. As it has been already established that periodontal health is affected by factors such as tobacco chewing or smoking and systemic conditions such as diabetes, leukemia, hormonal disorders [15]the individuals with these factors were also excluded from the study.
In the present study, the plaque and gingival indices were chosen because it gives mean score for each individual and it is comparatively easy to assess changes in longitudinal study [16]. In the present study, no statistically significant differences between the PLI scores of the study and the control groups in the first three examinations in contrast to the findings of Taani., et al. [17] where significant difference was detected in PLI score among pregnant and non-pregnant women. While the significant difference in PLI score was observed at the fourth examination for the study group than in control group and the probable reason could be the study group after delivering the baby had more focus towards the baby care and would have neglected their own oral hygiene. These findings are in contrast to Tilakaratne., et al. [3] and Sillness and Loe [18] where no significant difference in the plaque index scores was obtained during pregnancy and post partum.
The results of the present study revealed that the pregnant women exhibited significantly higher levels of gingivitis during the second trimester. The above findings are in agreement with studies of Cohen., et al [19], Arafat., et al. [11] and Samant., et al. [20] but differs from that of Loe and Sillness [21] who observed maximum at third trimester.
No significant difference was obtained in the scores of DMFT between groups which is in contrast to the study by Rakchanok., et al. [4] and Saurabha., et al. [22] where the pregnant women were more likely to suffer from dental caries. OHRQoL is taken as an important parameter to assess the impact of these oral health problems on their quality of life during three trimesters of pregnancy and post partum. The present study showed the mean scores of OHIP -14 for each fourteen questions and its seven dimensions for both the groups as well as overall mean score. The significant difference was found in the scores for question about taste sensation, amongst the groups in the first visit in line with the study done by Steven., et al. [23]. The most likely explanation for this could be that during first trimester of pregnancy, there is an abnormal taste sensation due physiological change.
Highest scores of OHIP-14 were presented in physical pain dimension in pregnant women. This finding is similar to the study conducted by Acharya., et al [6], Moimaz., et al. [24] and Lu., et al [25]. Also, study conducted by Olievera., et al. [26] and Wandera., et al. [27] showed that oral pain affects quality of life during pregnancy. The tool used in these two studies was Oral Impact Daily Performance (OIDP) which assess the effects of oral pain on their normal daily activities whereas the present study used OHIP14 as an instrument to assess the oral health related quality of life, so interpretation should be done cautiously.
Also, there was a significant higher score in the pregnant group for the question 5 (self conscious about their mouth) in the second trimester. The possible explanation could be many women experience gingival bleeding and gingival sensitivity in teeth more during pregnancy.
The present study reveals that there was no significant difference in overall OHIP score for pregnant group and control group and the mean OHIP-14 score ranges from 3.25 to 3.59 during pregnancy which is much lower than the study conducted by Moimaz., et al. (10.6) [24], Lu., et al. (7.92) [25], Acharya., et al. (7.0) [6], George., et al. (6.8) [28] and almost near to the scores study by Lamarca., et al. (3.8) [29]. The probable reason for the lower overall OHIP14 score as compared to other studies could be to some extent the social desirability bias while responding to OHIP -14 questionnaire and could be one of the limitations. But, the major strength of our study is the analysis of each dimension of OHRQoL not only in all the trimesters but also at time of post-partum and hence, its findings cannot be equated with the other studies in toto.
Although the present study concluded that there was no significant difference in overall OHIP-14 score between the pregnant and non-pregnant women but its longitudinal assessment revealed a significant positive impact during first and second trimesters in the three dimensions of Oral Health Impact Profile. This study provides an evidence to incorporate the oral health component as an urgent need in already existing maternal and child health care programs. In India, social, cultural and economic factors play a significant role in inhibiting women from seeking health care facilities. The main barrier in seeking dental care during pregnancy was fear for the safety of child. Hence, it is recommended that educating the pregnant women on the importance of oral hygiene and visit the dentist during this period can have a major impact in improving their quality of life and making the experience more beautiful.
Authors declare conflict of interest as nil.
Copyright: © 2019 J Kittu., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.