Fatma G Ashlak1, Fowziya M Ali1 and Ahmed Abouserwel2
1Paediatric Dentistry, University of Benghazi, Libya
2Dental Board, Hywel Dda University, UK
*Corresponding Author: Ahmed Abouserwel, Dental Board, Hywel Dda University, UK.
Received: October 07, 2024; Published: October 31, 2024
Citation: Ahmed Abouserwel., et al. “Parents’ Knowledge and Attitudes in Oral Health in their Down’s Syndrome Children in Benghazi, Libya". Acta Scientific Dental Sciences 8.11 (2024):83-91.
The primary objective was to evaluate parents' knowledge and attitudes toward oral health in their children with Down syndrome in Benghazi.
Subjects and Methods At rehabilitation facilities that treat individuals with Down syndrome (DS), a cross-sectional study on the parents of their children receiving services from government and non-government institutions in Benghazi was conducted. Two sections of a self-generated questionnaire with 27 questions about the patient's medical history, sociodemographic, and dental health treatment were utilized to gather data. The University of Benghazi’s Research Committee at the Faculty of Dentistry provided ethical approval (reference number 086). Before the study began, all parents signed a consent form.
Results: Of the 102 questionnaires given to participating parents/caregivers of children with DS, 35 (34.3%) were female and 67 (65.7%) were male. Of the 60 individuals with DS, 58.8% were boys and 41.2% were girls. Of the total participants, 52.9 percent were from the government sector and 47.1 percent were from the non-government sector for rehabilitative and educational services. Children with DS ranging in age from under five to over fifteen were included in the study. Sibling child order: first 20.6%, second 27.5%, third 13.7%, and higher 39% 21.6 had thyroid gland problems, 7.8 had heart disease, and 28.4 had diabetes. Of them, 62% did not visit a hospital or obtain medical attention during the year. A daily toothbrush is used by 52% of participants once a day, 21% irregularly, and 27.5% twice a day or more. Only 19% of them used rotating toothbrushes; most used manual ones. In a rehabilitation institution, most people (96.1%) received education regarding oral health. In the preceding six months, 20.6% of respondents visited a dentist, 63.7% did so once a year, and 15.7% never did. Visiting dentist to get an examination in 37.3%, trauma (22%), toothache (23%), and tooth-decay (19%).
Conclusion: Parents of children with Down syndrome need educational programs that promote positive attitudes and increase knowledge about oral health care. It is important to emphasize that parents should receive high-level information and guidance on how to care for their affected children
Keywords: Down Syndrome; Oral Health; Children; Parents’ Knowledge; Attitude
DS: Down Syndrome; CHD: Congenital Heart Disease; GI: Gastrointestinal; SPSS: Statistical Package for the Social Sciences
John Langdon-Down first recognized Down syndrome (DS), an autosomal chromosomal disorder, in 1866. It is one of the anomalies in life that arises from the trisomy of chromosome 21. DS affects different groups differently (1 in 319 to 1 in 1000 live births), and it is more common in older mothers. In neonates with DS, up to 50% may get CHD [1]. Since DS affects numerous systems, it is linked to a variety of clinical disorders. Numerous manifestations and signs are present in these people, including neurological traits, congenital heart defects, (GI) abnormalities, abnormalities, distinctive facial features, and intellectual and developmental difficulties [1-4]. The most anatomical feature of DS, including the facial mid-third, is underdeveloped, creating a prognathic occlusal relationship, producing a hypoplastic maxilla with a high, short, and narrow palate, brachycephalic with a flattening of the cranial occiput, and the mandibular prognathism is mild or marked relative to the maxilla [5]. For children with Down syndrome, orofacial problems are a major concern. Children with DS occasionally have physical, mental, and structural abnormalities [5,6]. Neuro-behavioural and mental issues are more prevalent in children with Down syndrome (18% to 38%). Disorders characterized by disruptive behaviour, such as obsessive-compulsive disorders and attention deficit hyperactivity disorder (6.1%), conduct/oppositional disorder (5.4%), or aggressive behaviour (6.5%), are the most common issues. Over 25% of individuals with DS suffer from a mental illness, with major depressive disorder (6.1%) and violent behaviour (6.1%) being the most common. Of children with DS, 7% have an autism or autism spectrum disorder diagnosis [7]. Epilepsy is seen in 8% of children with DS, with 40% occurring in infancy and often presenting as infantile spasms. Alzheimer’s disease which is associated with DS appears later in life, not in childhood [8]. Additionally, it is crucial to provide children with DS with ongoing medical evaluations and screenings throughout their lives [9]. In addition to the immunological and psycho-emotional benefits, nursing is especially beneficial for children with Down syndrome because it stimulates the development of the oral motor system. For this reason, breastfeeding should be encouraged [10]. [Moreover, individuals with DS have unique oral health needs that are critical to their overall health and well-being due to a variety of physiological and medical characteristics. Dental health is directly impacted by many medical and physiological elements of DS, which can impact the quality of life for individuals with the condition and those who provide care for them [11]. However, because of their impaired oral motor function, children with DS can have problems with drinking, swallowing, and chewing. Overweight and overnutrition deserve serious attention in children with DS [12]. Modeer., et al. 1990 found that the prevalence of gingival inflammation, periodontal pockets (5 mm), supra- and subgingival calculus, and alveolar bone loss was measured in children (10-19 years old) with DS in comparison to an age- and sex-matched 39 control group and of the 71 children with DS participated in a clinical and radiological evaluation. Alveolar bone loss was noted around the incisors and first molars on intraoral radiography when the distance between the cementoenamel junction and the alveolar crest exceeded 2.0 mm. Alveolar bone loss was found in 39% of the children [13]. According to their mothers’ children with DS could have a variety of issues, including Mothers reporting that their children's overall mood was impacted by the painful behaviours they saw in them. Some moms claimed that their children cried out stopped laughing, and got furious, which was thought to be an indication that their children were experiencing tooth pain. Some moms mentioned that their infants were dribbling or drooling, while others said that their children's tongues were comparatively large or protruding when they were younger. Mothers stated that because of the early functional therapy interventions they received, these issues seemed to lessen as their child grew older and, in several cases, were nearly resolved [14]. A study on dental caries in individuals with DS found that only approximately 31% of the participants had parental assistance when brushing their teeth and that roughly 50% of people with caries and the other half are free of caries. Although 91% of persons experience physical and/or cognitive impairments when following the recommended dental hygiene procedures [15,16]. In contrast, periodontal disease is prone to being particularly aggressive in a patient with DS [11,16]. A comprehensive analysis of the evidence implies reduced caries in individuals with DS. Furthermore, gingivitis and periodontitis are more frequent in people with DS and are strongly associated. Oral function in DS is also affected resulting in speech, breathing, and eating problems. These findings underscore the necessity to implement targeted educational and awareness programs, along with specific intervention protocols, for the younger generations of individuals with DS, their families, and caregivers [17]. Previous studies have indicated that the parents did not have enough knowledge about the importance of regular dental examinations on oral and dental health (Kalyoncu, 2018). Furthermore, the oral hygiene of children with DS and the oral hygiene knowledge of their parents showed a notable and robust inverse association. Dental hygiene practices among DS children were influenced by parents' knowledge [18].
Subjects and Methods
The current study was planned to assess parental knowledge and attitudes toward oral health in their children with DS in Benghazi. A cross-sectional survey using a questionnaire for data collection of parents concerning the oral health status of DS children in Benghazi City. The current study's population consists of the government and non-government DS Association of parents in Benghazi city. Approval from authorities from Benghazi University was provided, and permission for participation was delivered to clinic principals. There were two sections to the questionnaire created for this study. The respondent's background information is contained in the first part and includes the work type, gender, age group, income, and employment of their parents. The second section of the questionnaire, which covers oral and dental hygiene practices, is the primary portion. It aims to ascertain respondents' overall knowledge and attitude toward oral health care. Version 25 of (SPSS) was used to analyse the data. Descriptive statistics were recorded through frequency and percentages. The chi-square test was used to compare differences in proportions with parents' knowledge and attitudes.
Table 1 displays that the majority (59.8%) of DS children in the survey were from the age group (10-14 years). However, the minority (7.8%) of children with DS are in the age group (less than five years). 58.8% of DS children were males, and 41.2% were females. According to the order of children with DS in the family, 38.2% of children were of order more than the third, followed by the second and the first child order, (27.5%) and (20.6%), respectively. In contrast, the minority of the children (13.7%) were of the third order in their families.
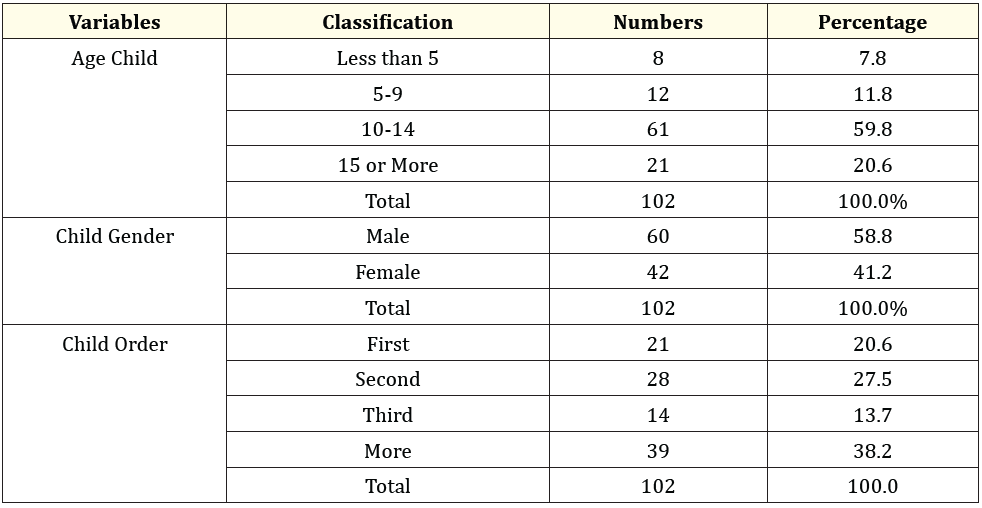
Table 1: Sociodemographic characteristics of DS children.
According to Table 2, more than half of the participants (52.9%, 54 out of 102) were from the public sector, whereas, (47.1%, 48 out of 102) were from the private sector. Table 1 also shows that most respondents (65.7%) were males, compared to 34.3% of females. The majority (71.6%) of respondents participating in the survey were aged less than 60 years. Regarding the income level, the majority (82.4%) have a moderate-income level, and the rest (17.6%) have a low-income level. the most frequent father occupation was an employee (43.1%), followed by free business (29.4%), while 27.2% were retired. Concerning the mothers' occupation, 52% of the respondents were housewives; 32.4% were found to be teachers, while 15.7% were employed. Regarding the father's education, 32.4% of parents have secondary level education, and 27.5% of parents have either preparatory or university level education, whereas, the respondents with primary level education were 12.7%, the minority of respondents participating in the survey. However, most mothers (37.3%) have a university education level, followed by 30.4% who have a secondary education level, while the rest of the respondents have preparatory and primary education levels, which were the minority of respondents participating in the survey.
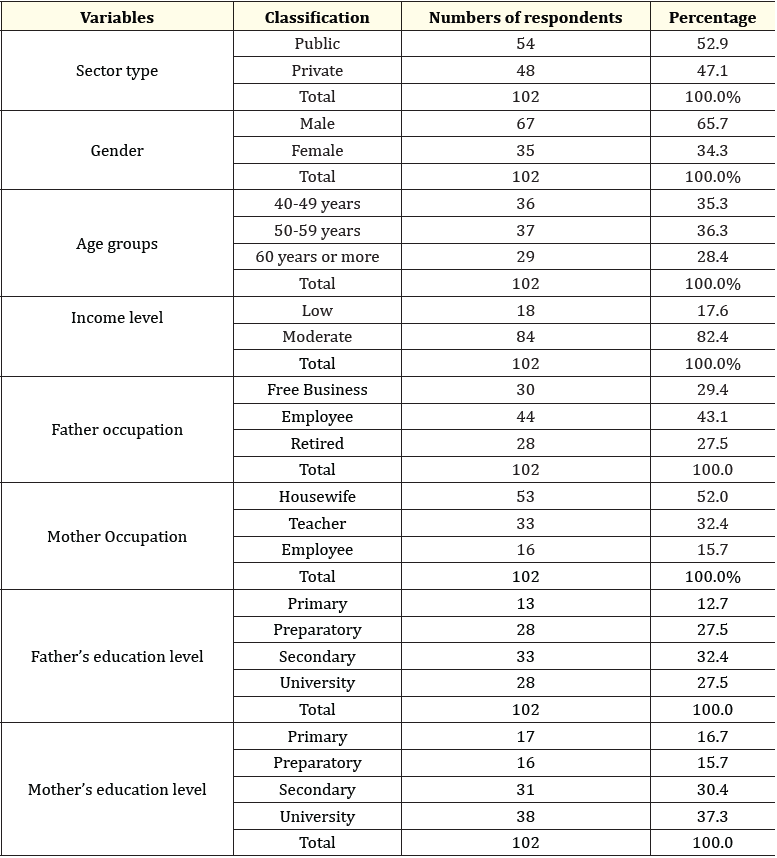
Table 2: Shows the distribution of DS child parents by age, gender, and socioeconomic level.
The majority of children (57.8%) have health problems, (Table 3). The majority of parents 62.7% reported that they had not been referred to a hospital in the preceding year, whereas 37.3% said they had.
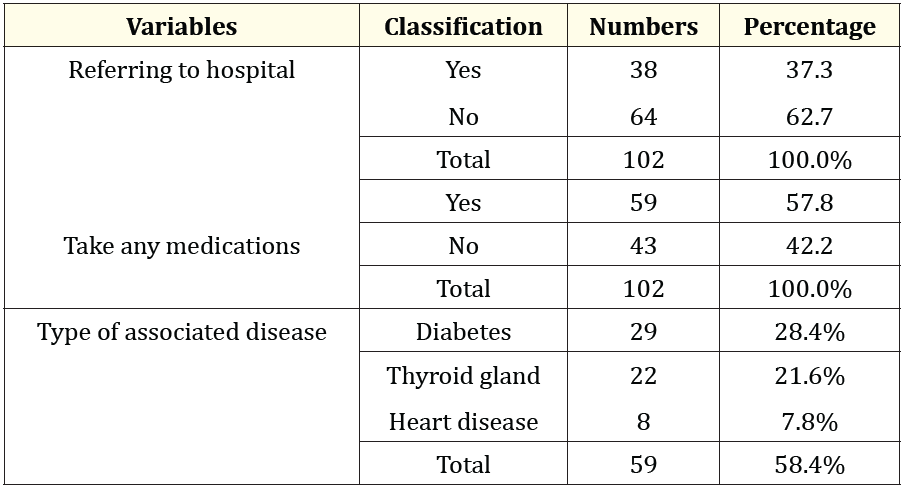
Table 3: Description of the samples according to the Down syndrome children’s health.
The age group of the parents who were brushing the children's teeth differed from one another in a statistically significant way (p < 0.05). Compared to parents in other age groups, parents 60 years of age or older were less likely to be supporting their children. However, the vast majority of them (52.9%) did not encourage or assist with their youngsters' tooth brushing. (Table 4).
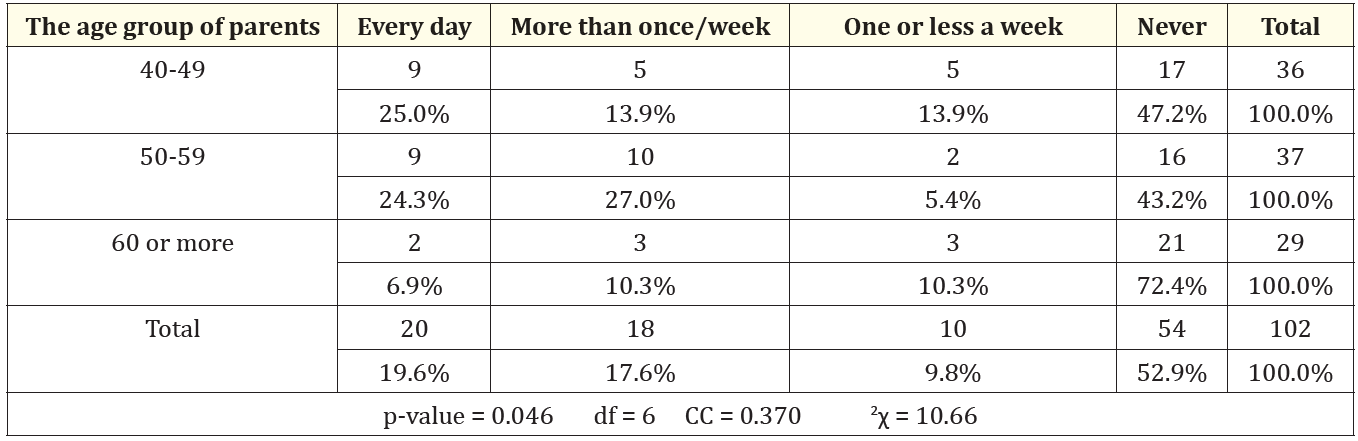
Table 4: Association between age groups of parents/ caregivers and supporting a child’s tooth brushing children.
‘*’ Statistically significant at 5%; ‘*’ CC: Contingency Coefficient
A statistically significant correlation was seen between the parents' age group and the number of times they took their kids to the dentist (p-value ≤ 0.04), suggesting that parents in the 50-59 age range were more likely than those in other age groups to take their children to the dentist. About taking their children to the dentist, the parents said that within six months, 20.6%, 63.7% within a year, and 15.7% never took them. In (Table 5).
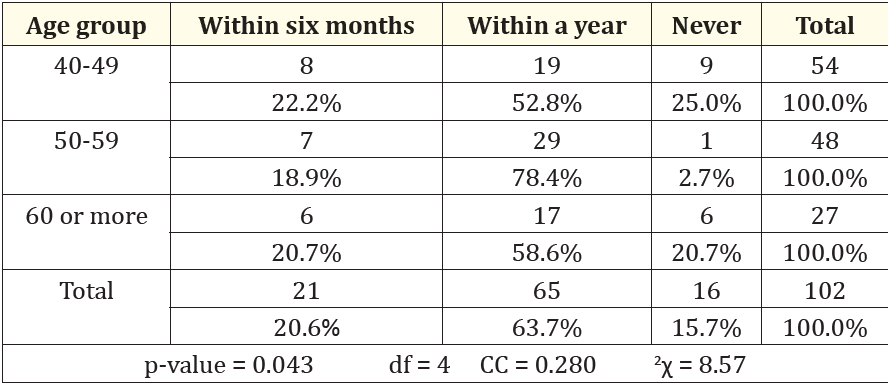
Table 5: Correlation between parent age groups and visiting the dentist with their children.
‘*’Statistical significant at 5%; ‘*’ CC: Contingency Coefficient
A statistically significant correlation was found between the parents' age group and the dental health care facility they got (p-value ≤ 0.002), suggesting that obtaining dental care from public health care was more likely to result in favourable outcomes than other forms of dental care figure 1.
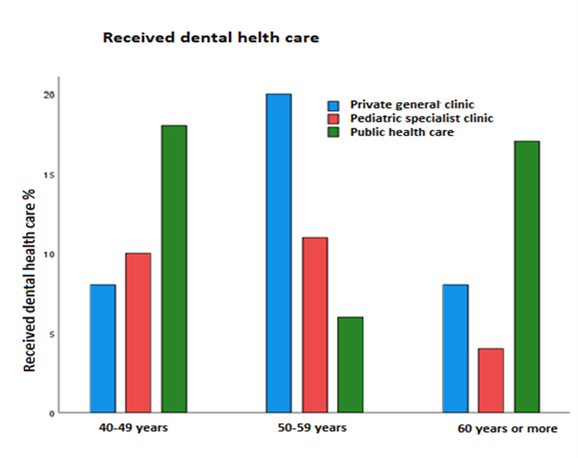
Figure 1: Association between age groups of parents and received dental health care facility.
Parents' gender did not significantly affect whether or not they helped their kids brush their teeth (p-value> 0.05). However, parents' gender did significantly affect what they thought were the most important qualities in a dentist (p-value ≤ 0.05). Of the parents, half (50.7%) of the male respondents chose to "involve the child in treatment," which was statistically significant more often than the female responses (Figure 2).
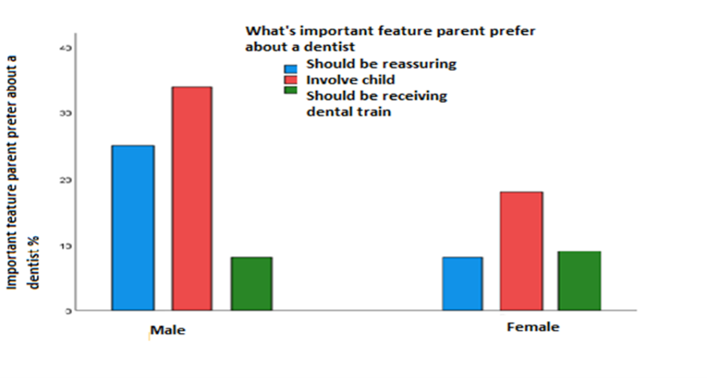
Figure 2: Association between the most important features of the dentists they prefer and the gender of parents.
The relationship between fathers' education levels and taking their children to the dentist was found to be statistically significant (p-value < 0.05). Fathers who completed secondary school and university had higher education levels associated with taking their children to the dentist than other fathers. However, there was no statistically significant correlation (p-value > 0.05) between the father's educational attainment and his assistance in brushing their children's teeth (Figure 3).
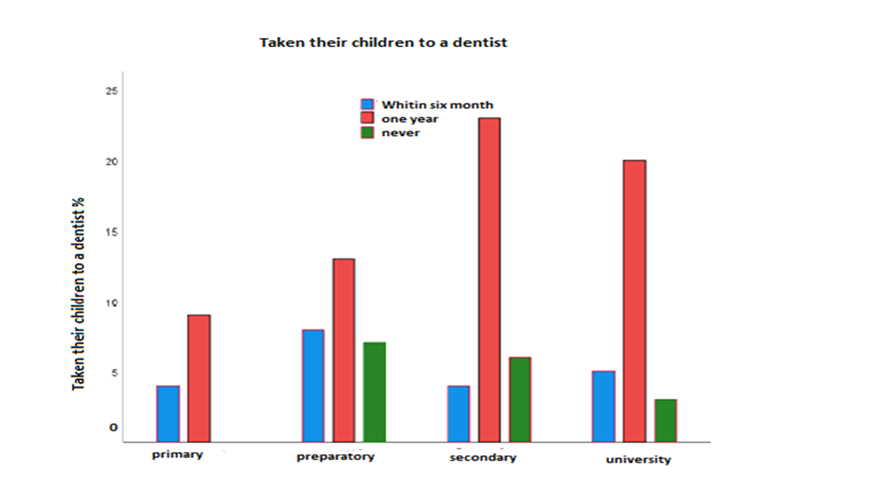
Figure 3: Association between the father's education level and taking their children to a dentist.
The mother's occupation and the oral health care facility their children received differed statistically significantly (p-value ≤ 0.04) and most of them sought public health care (Figure 4).
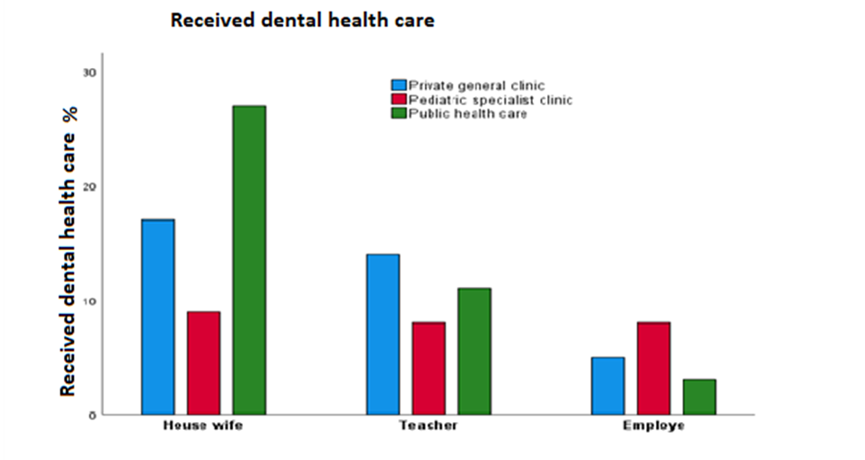
Figure 4: Association between mother's occupation and received dental health care facility for their children.
Children's dental health can be neglected because of a disability, a challenging illness, or restricted access to dental care. Parents should be required to receive education about proper oral hygiene for their children since it can greatly aid in the growth and development of their teeth. Several factors, including age, education, experience, economic and social status, the media, and the surrounding environment, may have an impact on parents' awareness of and ability to maintain their children's dental hygiene. The attitude and behaviour of their children will be greatly influenced by their parent's capacity to preserve their health. According to their mothers, children with Down syndrome could have a variety of issues, including Mothers reported that they saw signs of pain in their children and that this had an impact on the child's overall attitude. Others claimed that their children cried out stopped laughing, and got furious, which was thought to be an indication that their children were experiencing tooth pain. Some moms mentioned that their infants were dribbling or drooling, while others said that their children's tongues were comparatively large or protruding when they were younger. Mothers stated that as their youngsters grew older, these issues seemed to lessen and, in many situations, were nearly resolved again as a result of the early functional therapy [14,19]. Early professional treatment and daily care at home can mitigate their severity and allow people with Down syndrome to enjoy the benefits of a healthy mouth. Periodontal disease is the most significant oral health problem in people with Down syndrome. Children experience rapid, destructive periodontal disease. Consequently, large numbers of them lose their permanent anterior teeth in their early teens. Contributing factors include poor oral hygiene, malocclusion, bruxism, conical-shaped tooth roots, and abnormal host response because of a compromised immune system. Some patients benefit from the daily use of an antimicrobial agent such as chlorhexidine. Recommend an appropriate delivery method based on your patient’s abilities. Rinsing, for example, may not work for a person who has swallowing difficulties or one who cannot expectorate. Chlorhexidine applied using a spray bottle or toothbrush is equally efficacious. If the use of particular medications has led to gingival hyperplasia, emphasize the importance of daily oral hygiene and frequent professional cleanings. Encourage independence in daily oral hygiene. Ask patients to show you how they brush, and follow up with specific recommendations on brushing methods or toothbrush adaptations. Involve patients in hands-on demonstrations of brushing and flossing. Some people with Down syndrome can brush and floss independently, but many need help. Talk to their caregivers about daily oral hygiene. Do not assume that all caregivers know the basics; demonstrate proper brushing and flossing techniques. A power toothbrush or a floss holder can simplify oral care. Also, use your experiences with each patient to demonstrate sitting or standing positions for the caregiver. Emphasize that a consistent approach to oral hygiene is important caregivers should try to use the same location, timing, and positioning. Dental caries. Children and young adults who have Down syndrome have fewer caries than people without this developmental disability. Several associated oral conditions may contribute to this fact: delayed eruption of primary and permanent teeth; missing permanent teeth; and small teeth with wider spaces between them, which make it easier to remove plaque. Additionally, the diets of many children with Down syndrome are closely supervised to prevent obesity; this helps reduce the consumption of cariogenic foods and beverages [20]. This study assessed the views and comprehension of parents regarding the oral health condition of their children with Down syndrome who attended a rehabilitation centre, utilising data gathered from a sample of parents in Benghazi City, resulting in a response rate of 98.3%. The majority of fathers' education levels were secondary (32.4%), whereas the majority of mothers' education levels were university (37.3%), with the father's occupations being employed (43.1%) and housewife (52%). In contrast, in a study by Putri et al., 50% of participants had higher education (bachelor's or PhD degree), and 50% had only had secondary education (Putri, 2018). Similar to our study, another study reported that the majority of mothers (71.4%) were housewives [21].
The results indicate that some of the parents in the study group have a high education level. The study's findings indicate that most children with Down syndrome were male (58.8%), aged between 10 to 14 years (59.8%), and positioned higher than third in their family hierarchy (38.2%), similar findings were reported by Descamps et al., where the majority were male [22]. Our study found that the majority of children were not referred to a hospital during the previous 12 months (62.7%). According to a related report by Stensson., et al., (20%) of children had been referred to a hospital in the previous 12 months [23]. Our study found that most of the children used a manual toothbrush and more than half (52.9%) reported never helping their teeth. According to a related report by Schmidt., et al., (53.8%) of children with Down syndrome younger than 18 years most frequently used manual toothbrushes, (60.4%) stated that the children with DS in their home could brush their teeth without help [24,25]. Additionally, our study reported that (63.7%) of parents had taken their child to a dentist in the last years and answered the reason for visiting the dentist almost (37.3%) of the reason was for examination. The same finding in another study approximately half of the subjects from children with DS had visited a dentist within the previous year [26].
Regular visits to the dentist are very important for the prevention of oral diseases in disabled children and their parents for obtaining essential information about oral hygiene maintenance and dietary advice specific to their child’s disability from a dentist [23]. about the preferred dental visits and perceived obstacles to dental care for kids with special needs and their ability to get dental care in public dental facilities, private dentistry clinics, or specialised paediatric dental clinics in Benghazi. Most people favoured the field of public dental health. This study aimed to characterize the dental visitation patterns, assess accessibility, and pinpoint obstacles to dental care for children with DS. In our study, it was observed that most of the parents of children aged (50-59) years were statistically significantly more than other groups of children with DS taken their children to the dentist within the previous "one year". Another study by Syama et al. found that parents of disabled children visited the dentist more frequently (46%) in the past year than parents of normal developing children (40%) [27]. Furthermore, Difficulty in getting an appointment was the most common perceived barrier to dental care by parents of Down syndrome children and normal children (37.3%). Parents of disabled children considered difficulty in cooperation as a more important barrier to treatment (34.7%) than the parents of normal children (20.3%) [27]. Another study reported that 25% of respondents had difficulty finding dental care services for their DS child and 46.9% admitted that healthcare for their DS child took more time [28]. In the present study, most of the parents 52.9%) Never helped their children brush their teeth compared to another survey, researchers discovered that nearly 59.4% of parents helped their children brush their teeth [29]. Also, Alhaddad., et al. 2018 found a deficiency in knowledge and attitude towards DS individuals and nearly 59.5% indicated their willingness to help those with DS to lead regular lives [30]. while (95.8%) are willing to support their children in living a normal life [31].
In our study, it was found that most parents who had better education said that the one who trained their children in oral hygiene was the teacher. According to a study from 2015, the majority of information was obtained by "Dentists," while 20% of the parents of children with DS never received any oral hygiene advice [22]. Additionally, according to research by (Kalyoncu., et al., 2018), the majority of families (47.5%) learned about oral hygiene through dentists, while 18.4% did so from teachers. So it is important to emphasize the importance of daily oral hygiene and frequent professional cleanings. Encourage independence in daily oral hygiene. Ask patients to show you how they brush and follow up with specific recommendations on brushing methods or toothbrush adaptations. Involve patients in hands-on demonstrations of brushing and flossing. Some people with Down syndrome can brush and floss independently, but many need help. Talk to their caregivers about daily oral hygiene. Do not assume that all caregivers know the basics; demonstrate proper brushing and flossing techniques. A power toothbrush or a floss holder can simplify oral care. Also, use your experiences with each patient to demonstrate sitting or standing positions for the caregiver. Emphasize that a consistent approach to oral hygiene is important caregivers should try to use the same location, timing, and positioning. Dental caries. Children and young adults who have Down syndrome have fewer caries than people without this developmental disability. Several associated oral conditions may contribute to this fact: delayed eruption of primary and permanent teeth; missing permanent teeth; and small teeth with wider spaces between them, which make it easier to remove plaque. Additionally, the diets of many DS children are closely supervised to prevent obesity; this helps reduce the consumption of cariogenic foods and beverages [20].
Parents who participated in this study had some knowledge about the oral health of an individual with Down syndrome, but more than half of them did not have enough general knowledge and had difficulties finding oral healthcare. Furthermore, the findings of this study also revealed that almost all parents emphasize that there is a need for more high-level information and guidance and the need to improve the dental services available to individuals with DS. Also, parents need more attention to help their children in terms of supervising their oral health habits and providing dental care.
We would like to thank all parents and their children who gave their consent to participate in this study to enhance the results and Dr. Yousif Elgimati who assisted in the statistical analysis of this study data.
Copyright: © 2024 Ahmed Abouserwel., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.