Tofiq Bohra1* and Saurabh Shah2
1Senior Consultant and Unit Head at S L Raheja Hospital Mumbai, Oral and Maxillofacial Surgeon, Fellow - Cleft and Craniofacial Surgery, CCI, Fellow Arthroscopy and Total Joint Replacement, USA, Certification - Pain Management and Interventional Pain Society,
British Pain Society, India
2BDS, Pvt practice at Ghatkopar Mumbai. PGDMLS, Certification Summer School on
TMDs-University of Vienna, Member of American Association of Orofacial Pain -USA, Fellow of Orofacial Pain, Rosemann University -USA. Accredited Member of IAACD, India
*Corresponding Author: Tofiq Bohra, Senior Consultant and Unit Head at S L Raheja Hospital Mumbai, Oral and Maxillofacial Surgeon, Fellow - Cleft and Craniofacial Surgery, CCI, Fellow Arthroscopy and Total Joint Replacement, USA, Certification - Pain Management and Interventional Pain Society, British Pain Society, India.
Received: September 11, 2024; Published: September 30, 2024
Citation: Tofiq Bohra and Saurabh Shah. “TMJ Arthroscopy a Clinical Guideline". Acta Scientific Dental Sciences 8.10 (2024):88-93.
Temporomandibular Joint (TMJ) Disorders specifically Internal Derangement are a significant yet often overlooked category of health issues that can profoundly affect a person's quality of life. Despite their prevalence, these disorders remain under-diagnosed and misunderstood, creating a gap in effective treatment and patient care. The complexity of TMJ Disorders, coupled with their ability to mimic other conditions, often leads to a prolonged and frustrating journey for those seeking relief. There has been a long standing debate over the treatment of TMJ Disorders because of reduced treatment options. TMJ Arthroscopy in recent years has emerged as an effective mode of initial management of TMJ Internal Derangement in a minimally invasive method with minimum risk to Facial nerve and fewer complications. This article describes the conceptual guideline for the fresh Maxillofacial Surgeon to effectively perform TMJ Arthroscopy.
Keywords:TMJ Disorders, TMD, Minimally invasive surgery
Temporomandibular Joint (TMJ) arthroscopy is a minimally invasive surgical procedure used to diagnose and treat disorders of the temporomandibular joint. Disorders in this joint can lead to pain, dysfunction, and restricted movement. For cases which do not respond to the conventional and conservative treatments like intra occlusal orthopaedic splints, physiotherapy, rest and diet modification arthroscopy plays an intermediate role providing relief to patients without the need of open joint surgery.
Cases most routinely selected for arthroscopy are those refractory and not responding to conservative treatment. These include intracapsular disorders like disc displacement without reduction with restricted mouth opening, patients with pain score above 7, having difficulty in chewing regular food and those whose routine life is affected by TMJ pain.
Pre surgical blood work up of routine CBC, ESR, CRP, ANA, Anti CCP and Rh factor along with standard presurgical anaesthetist and medical clearance is taken
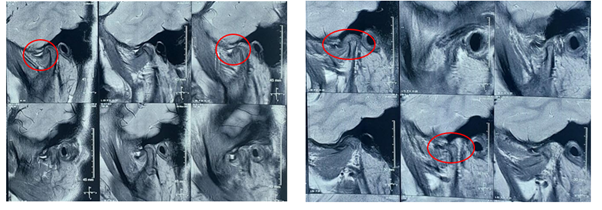
Figure a
Due to the severity of symptoms and lack of improvement with conservative management, the patient was scheduled for bilateral level 3 TMJ arthroscopy.
Considering her growing age, arthroscopy which is considered as bridge between conservative and surgical open joint treatment offers the best of both worlds, and with operator’s skill if level 3 is performed ligating disc also gives mechanical advantage of future disc displacement.
Under general anaesthesia, the patient was placed in the supine position with the head slightly extended. All standard asepsis protocols were followed such as draping, scrubbing surgical site with povidone- iodine
Basic armamentarium required for standard Level 3 Arthroscopy
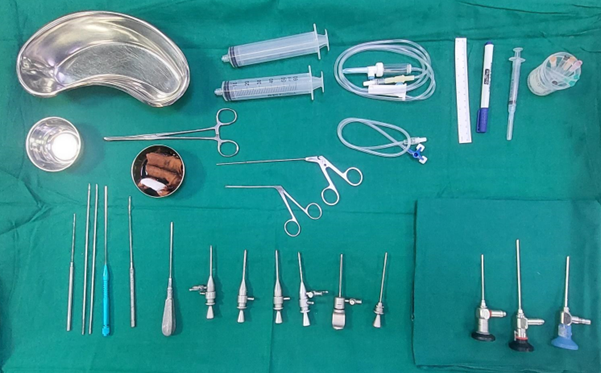
Figure 1: Tray setup for Arthroscopy Surgery.
In the pre-auricular region glenoid fossa is marked along with eminence, then the junction of zygomatic–temporal is palpated to locate the point of insertion in glenoid fossa. Once the position is confirmed along with condylar movements, condyle held in protruded position, the local anaesthetic intracapsular injection is administered. About 8 to 10 ml until backflow along with resistance is confirmed indicating complete joint insufflation. The direction of needle was aimed towards the glenoid fossa in superior joint compartment, anterior medial and superior direction aimed towards eminence.

Figure 2: Local Anaesthetic administration.
A TMJ arthroscopy sheath with sharp trocar is introduced to contact the zygomatic arch to raise the periosteum downward to further puncture the capsule and enter the superior joint space of TMJ, with continuous irrigation flow of about 50 ml per minute. This irrigation keeps the joint insufflated and makes the visibility and manoeuvrability of the instruments possible. Once the position is confirmed in the superior joint space, an outflow is established using a18 gauge needle to prevent extravasation of ringer lactate (RL) into fascial spaces around TMJ.

Figure 3: Port 1 with Scope and light source and outflow established.
Identifying important landmarks like medial drape, pterygoid shadow, articular eminence, anterior Recess, and articular disc, the damage is assessed and evaluated (Figure 4). Huge perforation was noticed in the retrodiscal area which was the main cause for pain as it was stretched between the bony surfaces as disc was placed anteriorly (Figure 5).
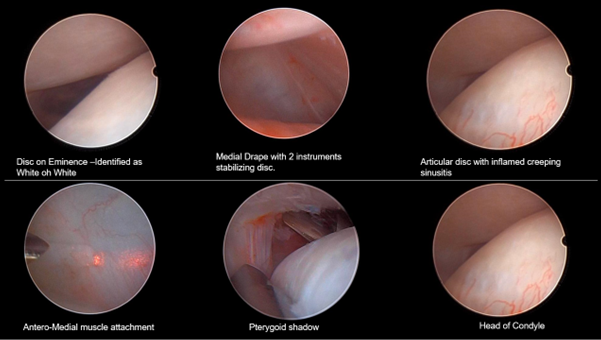
Figure 4: Various landmarks and tissue representation visible in arthroscopy.
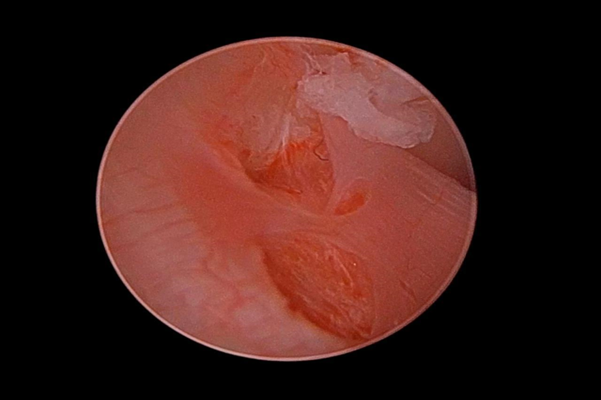
Figure 5: Tear visible in retrodiscal areas which was placed between the bony articular surfaces.
Once the landmarks and damage to the soft tissues is assessed, a laser myotomy is done with help of Holmium-YAG laser to release the superior lateral pterygoid muscle pull on disc antero-laterally (Figure 6). This procedure helps by releasing anterior disc pull that resists disc displacement.
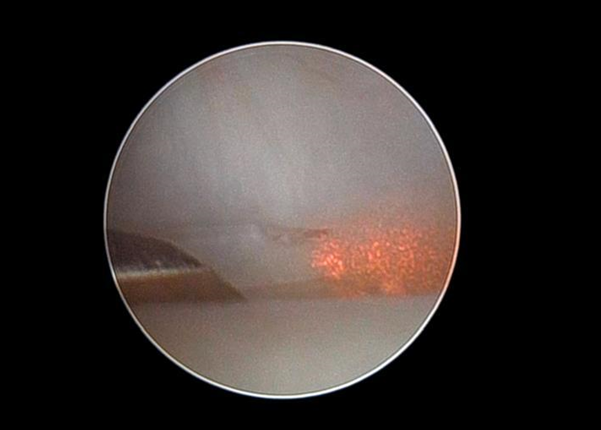
Figure 6: Laser myotomy releasing the anteromedial pull of superior lateral pterygoid muscle.
After myotomy, a third port which is an 18-gauge spinal needle is secured which passes through the disc from inferior joint space and is visualised under the scope. A 2-0 PDS suture is passed through this port and is retrieved via the fourth port using grasper forceps which is then passed subcutaneously using a suture needle in front of the tragus in order to anchor the disc in position.
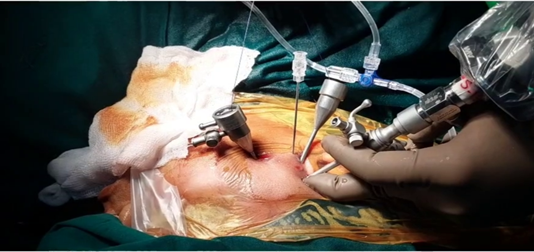
Figure 7: 3 Port access holes and 1 Spinal needle along with 2-0 PDS suture.
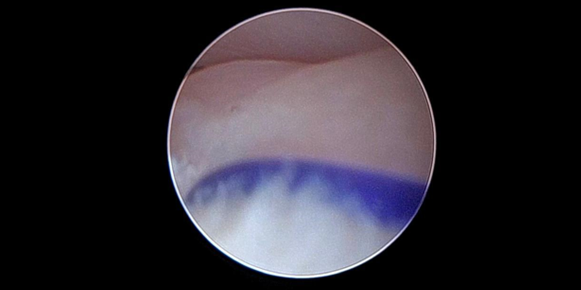
Figure 8: Suture in situ - holding the disc on the condyle head firmly.
Once the suture is ligated subcutaneously finally under vision kenacort (Triamcinolone acetonide 4mg) is injected under vision into the superior joint space, as an additional intra-articular anti-inflammatory treatment.
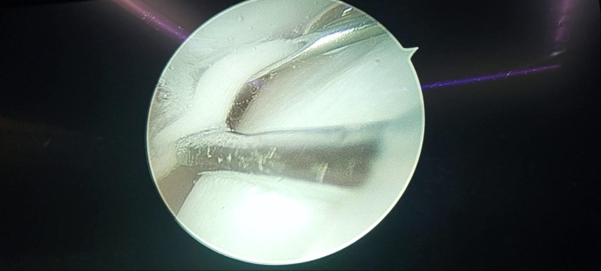
Figure 9: Colloid of kenacort injection under vision injected in superior joint space.
Once the above-mentioned procedures i.e. – Manual disc reduction, Laser myotomy, suture anchorage and kenacort injection- are done all instruments are retrieved and port openings are examined and rarely and port closure sutures are required making arthroscopy procedure very minimally invasive and scare free.
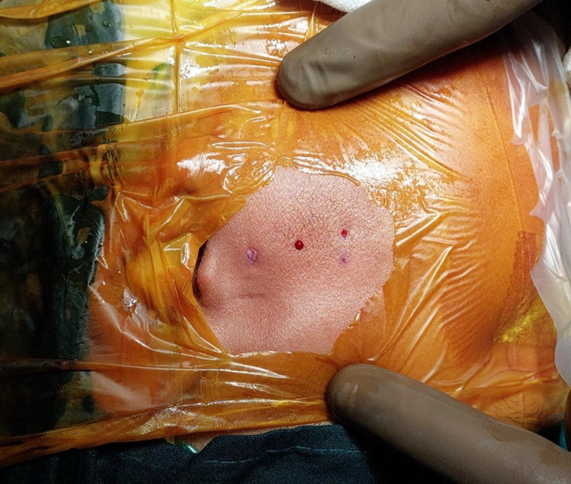
Figure 10: Post surgical port wounds - Minimally invasive and scare free procedure.
Following surgery, the patient was monitored closely for any signs of complications, including hematoma formation, infection, or neurovascular injury. Postoperative rehabilitation from the 3rd day included gentle jaw exercises, physical therapy of mouth opening of minimum 3 fingers, and analgesic medications to manage pain and swelling.
Post 10 day follow up, pain and function are evaluated and the patient is referred for intra oral orthopaedic appliance/splint which helps in joint healing, load management, managing para functions like Sleep bruxism /daytime clenching and any occlusal inferences if any. The patient is closely monitored for a period of 3 months with monthly intervals with respect to splint, pain and daily routine function.
At the one-month follow-up, the patient reported significant improvement in symptoms, including increased mouth opening and decreased pain. Physical examination revealed resolution of crepitus and improved joint function bilaterally.
Thus, an inclusive approach along with intra oral appliances and arthroscopy shows promising results.
Long-term follow-up will be essential to assess the durability of the surgical outcome and monitor for any recurrence of symptoms.
Tmj Arthroscopy should be considered as first line of surgical modality for treating TMJ osteoarthritis (OA Bilateral level 3 TMJ arthroscopy along with Splint therapy is an effective surgical intervention for the management of chronic TMJ disorders refractory to conservative treatment. Early diagnosis, appropriate patient selection, and meticulous surgical technique are essential for achieving favourable outcomes and improving patient quality of life.
Copyright: © 2024 Tofiq Bohra and Saurabh Shah. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.