Vishnusripriya J1*, Anil Melath2, Nanditha Chandran3, Hemalatha DM1, Fathima UM4 and Faby Ashraf4
1Senior Lecturer, Department of Periodontics, Mahe Institiute of Dental Sciences and Hospital, India
2HOD, Department of Periodontics, Mahe Institiute of Dental Sciences and Hospital, India
3Reader, Department of Periodontics, Mahe Institiute of Dental Sciences and Hospital, India
4Final Year BDS Student, Department of Periodontics, Mahe Institiute of Dental Sciences and Hospital, India
*Corresponding Author: Vishnusripriya J, Senior Lecturer, Department of Periodontics, Mahe Institiute of Dental Sciences and Hospital, India.
Received: August 28, 2024; Published: September 27, 2024
Citation: Vishnusripriya J., et al. “A Revisit of Non-Carious Cervical Lesions". Acta Scientific Dental Sciences 8.10 (2024):72-79.
Hard tissue loss in the cervical regions of teeth is a common and complex dental condition known as noncarious cervical lesions (NCCLs). In contrast to caries, NCCLs are brought on by a number of variables, such as occlusal tension, friction, and acid erosion. The current understanding of NCCLs, including their origin, clinical manifestations, and diagnosis, is reviewed in this article. We talk about how crucial it is to pinpoint the underlying causes and create individualized preventative and treatment plans. A number of therapeutic alternatives are also investigated, such as root covering surgery and adhesive restorations. The purpose of this article is to improve patient outcomes by giving dental professionals a better understanding and management of NCCLs, a complex disorder
Keywords: Non Carious; Abrasion; Erosion; Abfraction; Management
Dentists frequently encounter the problem of hard tissue loss at the cementoenamel junction (CEJ) in the course of their clinical work. These can have a variety of shapes and are referred to as non-carious cervical lesions. It is possible to observe enormous wedge-shaped defects, wide lesions that are scooped out, or shallow grooves. The labial, lingual/palatal, or proximal surfaces of the teeth may sustain these lesions [13]. To avoid more harm and to keep the current lesions from getting worse, it is critical to comprehend the underlying causes of these lesions. If the underlying causes of these lesions are not addressed, treatment will not be long-lasting. The most often mentioned reasons for cervical lesions include dental flexure, abrasion, and erosion. Hard tissue loss that is chemically caused and does not include germs is called dental erosion. It is typically brought on by tissues dissolving in acid. Conversely, abrasion refers to the erosion of tooth structure caused by external mechanical forces, with brushing being the main contributor. Another mechanism that might result in the loss of dental hard tissue is tooth flexure [7,8]. Although cervical lesions can develop anywhere in the dental arch, they are most frequently observed on teeth that are not molars. Lesions that are angular are more common than those that are rounded. It is believed that the lesion's shape depends on what caused it [1,6,9,11,12]. Determining the best course of action for treatment requires an understanding of the etiology of cervical lesions.
The non-carious cervical lesion (NCCL) is when there's a loss of tooth tissue at the neck of the affected teeth, but it's not related to tooth decay. It's been studied by many researchers since way back in 1908.
Erosion is when the hard dental tissues slowly get worn away due to chemicals, not bacteria. The smooth surfaces of our front and premolar teeth are particularly vulnerable to this when we consume acidic foods and drinks. It can cause the tooth tissue to erode. Interestingly, even our back teeth can be affected if someone regurgitates stomach acid. Being aware of these factors can help us take better care of our teeth. However, when it comes to erosive lesions, the location alone isn't a reliable predictor of the cause. Instead, researchers have found that the titratable acidity of a substance is more important than its pH in terms of tooth tissue erosion. For example, even though orange juice has a higher pH than cola, orange juice with a high titratable acidity can actually cause more erosion than cola [15-20].
Nowadays, due to better working conditions, exposure to airborne acids in industries like chemicals and metals is rare and not a common cause of erosive non-carious cervical lesions (NCCL). However, other activities, such as frequent swimming in chlorinated pools, have been more recently identified as a cause of erosion. There's also a condition called the "voluntary reflux phenomenon" that affects stressed individuals who find comfort in regurgitating and holding stomach contents in their mouth before spitting or swallowing it. This can lead to erosion of the tooth surfaces near the retained vomit, particularly in the lower premolar and permanent molar teeth [15]. The prevalence of these cervical erosion lesions isn't well-documented, but a study from 1949 found that 27% of the patients they examined had tooth tissue loss on the facial surfaces due to erosion. They also observed that the prevalence and severity of erosion lesions increased with age, with more lesions found in upper teeth compared to lower teeth, and the first premolar teeth being most commonly affected. Acids play a significant role in the etiology of these lesions [15,17].
Researchers have been studying the relationship between the quantity and quality of saliva and dental erosion. Some studies suggest that the citrate content of saliva may be linked to the severity of erosion. However, there are conflicting findings, as some studies did not find a significant difference in citrate content between patients with erosive lesions and those without. Additionally, an in vitro experiment found that pyrophosphate, a natural calcium chelating agent, was present in salivary debris from individuals with erosion but not in controls. However, it’s worth noting that in vitro experiments may not perfectly reflect real-life conditions [37-39]. Saliva plays an important role in rinsing away and neutralizing acids that can cause tooth erosion. When there is low salivary flow, it can increase the risk of dental erosion. Studies have shown that individuals with low unstimulated salivary flow rates have a higher risk of developing erosive lesions. Additionally, individuals with conditions like anorexia and bulimia may experience dry mouth (xerostomia) and have saliva with reduced buffering and remineralizing capacity [33,34]. The ability of saliva to fix eroded tooth surfaces can be different for different people. From studies it’s found that even though the amount, pH value, buffering capacity, and calcium and phosphorus levels in saliva were similar for both cases and controls, the amount of mucin, which is a component of saliva, varied. This mucin might help prevent the calcium and phosphorus from sticking to the teeth and repairing any damage caused by brushing. But, we still don’t know exactly how calcium and phosphorus in saliva affect dental erosion [32,35-37]. Other factors within the body have been suggested to contribute to the development of cervical lesions. Bodecker proposed that the exudate from the gums could start the erosion process [29]. Kornfeld believed that disturbances in the pulp tissues could cause decalcification [30]. More recent theories suggest a connection between stressful occlusion (how the teeth come together) and the development of cervical lesions [31].
Abrasion is the ‘abnormal wearing away of a substance or structure by a mechanical process’ [16]. Toothbrush abrasion happens when a substance or structure wears away due to mechanical processes. In the case of non-carious cervical lesions (NCCL), tooth brushing has been identified as a possible cause. Factors like how you brush, how often you brush, the stiffness of your toothbrush bristles, and the abrasiveness of your toothpaste can all contribute to the development of these lesions. Research has shown that people who brush twice a day may have a higher frequency of cervical lesions compared to those who brush less often. It’s also been found that brushing horizontally can lead to more wear on the dentin compared to brushing in a longitudinal direction [21]. Interestingly, there seems to be a higher number of NCCL on the left side for right-handed individuals, and areas that are brushed first may have more abrasive lesions due to increased brushing force [22].

Figure 1: Erosion.

Figure 2: Abrasion.
Some experts have suggested that there might be other factors involved in the development of non-carious cervical lesions (NCCL) that we haven’t traditionally considered [23,25]. One idea is that the pressure from biting and chewing can actually cause the tooth to bend and flex, which can lead to damage to the enamel at the cervical region. This kind of damage has been given the name “abfraction” by Grippo [24]. There have also been studies that looked at how the enamel behaves under friction and found that there can be cracks and weaknesses in the enamel rods and the substance between them. This can make the enamel more vulnerable to damage. Additionally, the bond between the enamel and the underlying dentin in the cervical area is not as strong as in other parts of the tooth, which can further contribute to the formation of NCCL. Both enamel and dentin are strong under compression, but they’re not as good at withstanding tension forces [26-28].
Figure 3: Showing various degrees of tooth wear.
It’s interesting to note that there’s a connection between bruxism (teeth grinding) and cervical erosion. Teeth with wear facets on the crown, which can be caused by bruxism, often show signs of erosion at the cervical area as well. However, the exact explanation for this connection is still being studied [14].
On the basis of etiology
On the basis of clinical severity: in 1979 Eccles
Classification of abrasion
Each class can be further sub-classified to quantify the severity of the le It is as follows:
The Tooth Wear Index proposed by Smith and Knight is the most accepted index to categorize tooth wear in the cervical region, and it is as follows:

Figure 4: Showing tooth wear index.
Seen as well-defined semicircular or semilunar shape radiolucent defects in cervical level of the tooth.

Figure 5: Radiographic view of abrasion.
Seen as radiolucent defects on the crown with well defined or diffused margins.
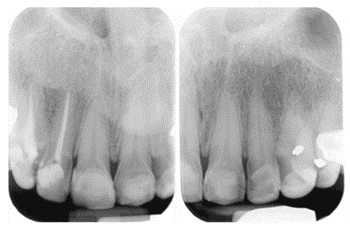
Figure 6: Radiographic view of Erosion.
In some cases, dental X-rays can help determine whether the lesions have affected the inner layers of the tooth, such as the dentin or pulp.
The main aim of preventive therapy for NCCLs is to prevent the lesions from getting worse and to make sure that restorations last. This involves counseling patients on behavior changes based on the cause of the lesions, such as aggressive brushing, faulty techniques, or abrasive toothpaste. Additionally, patients should be advised to avoid brushing immediately after an erosive challenge [49,50]. The success of treatment depends on how well the patient cooperates. If the erosion is caused by eating disorders or gastro esophageal reflux disease, it may require the involvement of a physician. Treating extrinsic factors is generally easier. During the diagnostic phase, making changes to or eliminating harmful habits can lead to consistent results [49]. If abfraction is suspected as the main cause, a conservative treatment option like using an occlusal splint may be recommended to reduce bruxism and non axial tooth forces. On the other hand, some experts believe that preventive management should include occlusal therapy for patients with parafunctional habits and occlusal imbalances. However, making irreversible treatments like occlusal adjustment should be carefully considered [49].
It’s crucial to assess the activity of NCCLs when planning treatment. The progression of these lesions can vary among patients, with some experiencing slow changes while others may have more rapid progression. That’s why it’s important to establish an individual monitoring protocol that takes into account factors like the severity of the lesions, the patient’s age, and any underlying causes or risk factors. For patients who are exposed to intrinsic acids or show signs of rapid progression, it’s recommended to regularly assess the activity of the lesions every 6 months during routine hygiene appointments. This helps ensure that appropriate treatment is provided in a timely manner. One way is by using standardized intraoral photographs and possibly study models to track changes over time. Another method is measuring the dimensions of the lesions (width/length) over time. With the advancements in digital dentistry, CAD/CAM systems can also be helpful in diagnosing NCCLs and monitoring their activity. V-shaped lesions tend to have higher stress levels concentrated at the top part of the lesion, while U-shaped defects distribute the stress over a wider area. As the lesions get deeper, the stress becomes more amplified at the deepest part. It’s important to keep in mind that patients with a heavy bite and jaw movement may need restorative treatment earlier for V-shaped lesions compared to U-shaped ones. Dentists usually prioritize restoring deeper NCCLs (around 1.5 mm) because they experience higher stress, leading to more noticeable progression.
Dentinal hypersensitivity is a common symptom in the early stages of NCCLs. If the lesions are small and shallow and don’t need restorative treatment, but the sensitivity persists, there are noninvasive options to try. You can find various at-home desensitizing agents on the market that work in different ways, like calming the nerves or blocking the dentin tubules. These agents come in toothpastes, mouthwashes, and chewing gums. After using them for a few weeks, see if the sensitivity improves. If it doesn’t, then it might be time to consider in-office treatment. Recently, they’ve introduced calcium- and phosphate-based systems for in-office use, which help reduce sensitivity and promote remineralization of the tooth surface. Clinical trials are needed to confirm the effectiveness of both systems [42,43]. When it comes to longer-lasting relief from dentin hypersensitivity, resin-based dental adhesive systems have shown promising results compared to home-desensitizing agents. These adhesive resins create a hybrid layer that effectively seals the dentinal tubules. Clinical studies have actually demonstrated the effectiveness of these adhesives for up to 6 months in managing dentin hypersensitivity [40,41,44].
When it comes to fixing NCCLs, there are a few situations where restorative treatment should be considered. These include having active cavities associated with the NCCLs, lesion margins that are located below the gum line and make it hard to clean, extensive tooth structure loss that weakens the tooth or exposes the pulp, persistent dentinal hypersensitivity that hasn’t been helped by non-invasive treatments, needing a prosthetic abutment for a removable prosthesis, or if patients have specific esthetic preferences. If a restoration is necessary, it’s best to do it in a minimally invasive way. Dentists often prefer using an adhesive system combined with a composite resin because it gives good esthetic results [45-47].
Adhesively restored NCCLs can actually do really well in the long run. There are a few things that affect how these restorations hold up over time. One important factor is the type of adhesive system used. Different adhesives have different levels of durability, so it’s important to choose the right one. Another key factor is the skill of the dentist. They need to take care during the entire process, from isolating the tooth to applying the adhesive and composite, and then finishing and polishing the restoration. And of course, ongoing maintenance is important too. It’s all about doing things right to ensure a successful and long-lasting result [46,48].
Periodontal therapy is required when non-carious cervical lesions are associated with considerable gingival recession and mucogingival defects. Root coverage procedures using free gingival grafts or connective tissue grafts are mainly chosen. Root coverage using non-grafting procedures like rotational and coronally advanced flaps or guided tissue regeneration are also done. Non-carious cervical lesions (NCCLs) can lead to gingival recession, which exposes root surfaces to the oral cavity. While it is feasible to place a composite restoration, the aesthetic outcome may not meet expectations. If the patient values aesthetics, the optimal treatment for addressing both non-carious cervical lesions and gingival recession, especially in the case of deep lesions, is a combined periodontal and restorative approach. In a combined restorative-surgical approach, it’s crucial to place the restoration before the surgical procedure for better visibility and the final restoration. To restore lost dental tissue due to wear, determining the maximum root coverage level is essential. The restoration should replicate the tooth crown contour and the lost CEJ at the root. Recent reviews suggest that combining a CAF (coronally advanced flap) with a CTG (connective tissue graft) offers the best outcomes for root coverage. However, there is still a lack of long-term evidence on the stability of this approach [50].
When it comes to diagnosing the causes of multifactorial NCCLs, it’s crucial for practitioners to consider a comprehensive medical and dental history, conduct an occlusal examination, evaluate the patient's diet and oral hygiene practices and the risk factors that contribute to the formation of NCCLs. When it comes to the treatment of NCCLs, a systematic approach is essential. This involves problem identification, diagnosis, removal of the underlying causes, monitoring, and, if necessary, treatment. Special attention should be given to the preventive phase, as It directly impacts the longevity of restorative treatment. It’s also important for the dentist to have a high level of skill and follow a meticulous operative procedure to maximize the lifespan of the treatment rendered.
Copyright: © 2024 Vishnusripriya J.,et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.