Nicolás Ibáñez-Ballesteros1*, Diego Robles-Zamorano2, Javier Orlando Botello-Romo2, Paulina Perez-Guzman1, Hernán Castillo-Cubillos3 and Juan Pablo Mendoza-Tapia2
1Dental Surgeon, Private Practice, Universidad Diego Portales, Santiago, Chile
2Dental Surgeon, Private Practice, Universidad Andres Bello, Santiago, Chile
3Dental Surgeon, Private Practice, Universidad Autonoma, Temuco, Chile
*Corresponding Author: Nicolás Ibáñez-Ballesteros, Dental Surgeon, Private Practice, Universidad Diego Portales, Santiago, Chile.
Received: September 19, 2024; Published: September 27, 2024
Citation: Nicolás Ibáñez-Ballesteros., et al. “Surgical Management of Frontal Sinus Fractures. Narrative Review". Acta Scientific Dental Sciences 8.10 (2024):63-67.
Frontal sinus fractures are relatively rare, accounting for 2% to 15% of facial fractures in different series. Frontal sinus fractures occur mostly as a result of high-energy trauma. Inadequate treatment can lead to serious complications even many years after the traumatic event. Treatment alternatives depend on the involvement of the anterior wall, nasofrontal duct and/or posterior wall is determined for each patient. The aim is to review the different treatment alternatives.
Objective: To describe the criteria to determine the most appropriate surgical management in patients with frontal sinus fracture.
Method: An electronic search was carried out in the following databases: PubMed, Science and SCOPUS, using as keywords: frontal sinus fracture - surgical treatment - obliteration cranialization using the Boolean operators AND/OR.
Keywords: Frontal Sinus Fracture; Surgical Treatment; Obliteration Cranialization; Nasofrontal Duct; Nasofrontal Sinus Fracture; Nasofrontal Duct
CSF: Cerebrospinal Fluid
Frontal sinuses are absent at birth, they begin to develop from 2 years of age derived from an evagination of the infundibular ethmoid cells of the frontal recess. They are not radiologically observed until 8 years of age, reaching adult size after 12 years of age. In 4% of people they are absent, in 5% they are unilateral and in 10% they are asymmetric. The frontal sinuses drain towards the middle meatus through the nasofrontal ducts which are located in the posteromedial region of the sinus floor [1] and descend obliquely downwards, inwards and backwards, flowing into the middle meatus, its length is approximately 15 to 20 mm, and its diameter is 2 to 4 mm. The nasofrontal duct is a complex formed by 3 distinct anatomical structures (infundibulum, orifice and frontal recess) that constitutes the drainage tract of the frontal sinus. It has a shape similar to an hourglass whose upper part is the frontal infundibulum located on the floor of the frontal sinus, where it narrows with a medial and posteroinferior inclination; then there is the frontal orifice or ostium in the direction of the ethmoid, it is the narrowest part of the tract and in the lower part is the frontal recess with an inverted funnel shape [2].
Sagittal view schematic of the frontal sinus and adjacent structures.
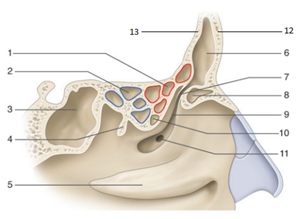
Figure 1: 1. Suprabullary cellae; 2. Posterior ethmoid cellae; 3. Sphenoid sinus; 4. Tail of middle turbinate; 5. Inferior nasal turbinate; 6. Frontal sinus; 7. Nasofrontal duct; 8. Uncibular canal; 10. Ethmoidal bulla; 11. Natural ostium of maxillary sinus; 12; 12. Anterior wall of frontal sinus; 13. Posterior wall of posterior sinus
The average volume of the adult frontal sinus is about 5 cm3. The frontal sinuses border posteriorly with the cribriform lamina, dura mater and frontal lobes. Inferiorly with the orbital roof [1-3]. The frontal sinuses are lined by the sinus mucosa, which is continued by the sinus mucosa of the ethmoid cells and the nasofrontal ducts that drain fluids from the frontal sinuses to the middle nasal meatus [1]. This mucosa is characterized by the presence of vascular nests of Breschet, venous drainage points which, on the one hand, can cause intracranial dissemination of infections and, on the other hand, can lead to the formation of mucoceles if the mucosa covering them is not adequately removed [4].
Axial and sagittal CT image of brain.
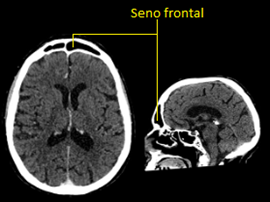
Figure 2: Brain CT image showing the frontal sinus and its proximity to the brain
Frontal sinus fractures are relatively infrequent, representing in different series from 2 to 15% of facial fractures [5]. Frontal sinus fractures occur as a result of high energy impacts with a blunt object, generally as a consequence of traffic accidents, robbery aggressions or during fights, so they are frequently observed in polytraumatized patients and with other facial fractures [6]. There are numerous classifications proposed for frontal sinus fractures, but in general it can be said that it is essential to assess the involvement of the anterior wall, the posterior wall and/or the nasofrontal canal [3].
An electronic search was performed in the databases: PubMed, Science and Scopus, using as keywords: frontal sinus fracture - surgical treatment - obliteration cranialization using the Boolean operators AND/OR. Inclusion criteria: study less than 15 years old, Spanish or English language, open access. Exclusion criteria: studies older than 15 years, language other than Spanish or English, without open access, systematic reviews. Critical reading of titles and abstracts was performed, and those that presented significant evidence were included.
Twelve articles dealing with the subject were found, from which the most relevant information was rescued, with the aim of providing a simple text to understand.
The treatment of frontal sinus fractures is controversial, it is important to consider that an inadequate treatment of these fractures can lead to serious complications, mainly of infectious type, even many years after the trauma [4]. This type of fractures can only compromise the patient's esthetics. In case of affecting the frontal sinus drainage, it can cause recurrent frontal sinusitis. A fracture of the posterior wall with involvement of the dura mater may allow bacteria to enter the brain, which may lead to meningitis. If the fracture compromises the barrier between the frontal sinus and the brain, cerebrospinal fluid may leak, which can lead to persistent headaches and increase the risk of meningeal infection [7]. On more complex occasions air may leak into the cranial cavity generating a pneumocephalus (air in the cranial cavity) [8], and an obstruction of the frontal sinus flow may lead to the formation of a mucocele [9], which is an accumulation of mucus that may expand and cause damage to surrounding structures.
Linear anterior wall fractures that are not associated with a nasofrontal canal lesion can be managed without surgical intervention. The same conduct should be followed in cases of slightly displaced fractures (less than 2 mm) in which the esthetic sequelae are minimal. In cases in which the fracture compromises the patient's esthetics, generating an evident deformity, it is necessary to reduce the fracture and perform the corresponding osteosynthesis [4].
When a lesion of the nasofrontal duct is suspected, a canal obliteration can be performed [10]. In frontal sinus obliteration, before reducing and fixing the bone fragments, it is essential to resect absolutely all the mucosa of these fragments, the duct and the sinus, and it is also advisable to mill the sinus walls to eliminate the mucosa that may remain in the vascular nests of Breschet.
Different materials have been proposed for obliteration with satisfactory results, both autologous and synthetic. Among the autologous materials (fat, muscle, bone), the advantages of calotte bone chip are that it is easy to obtain, it can be combined with other alloplastic materials and it allows an adequate radiological follow-up with CT, since it shows bone density in the radiological image, facilitating the early detection of complications such as mucoceles, fistulas or abscesses [11].
Filling of the frontal sinus.
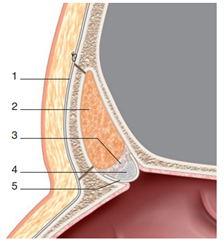
Figure 3: 1. Sutured periosteum; 2. Fat; 3. Biological adhesive; 4. Bone graft; 5. Pericranial or aponeurosis graft.
On the other hand, as an alternative to obliteration, some authors advocate preserving the functionality of the sinus in order to minimize the incidence of infectious complications. For this purpose, they resort to tutoring the nasofrontal duct by using a plastic drainage tube, which has to be left in place for a minimum of 30 to 40 days. However, up to 30% of failures due to stenosis of the nasofrontal canal have been described using this technique [2].
If the fracture of the anterior wall is displaced and no lesion of the canal is suspected, it should be reduced and fixed, complemented with bone grafts if necessary [6]. But if canal injury is suspected, it is necessary to complete the treatment with canal and sinus obliteration or canal tutoring.
Without esthetic compromise with or displacement less than 2 mm.
Esthetic compromise
Without compromise of frontal sinus drainage
With compromise of frontal sinus drainage
Regarding posterior wall fractures, in those linear fractures in which there is no CSF fistula, the attitude can be conservative, reevaluating the appearance of fistula.
When they are displaced and comminuted fractures, the ideal is to cranialize the sinus after completely eliminating the posterior wall fragments, repairing the dural defects (by means of direct suture or dura mater patches), obliterating the nasofrontal ducts and sealing the anterior cranial fossa with a galea-pericranium flap [10]. This is an attempt to isolate the intracranial space to avoid the appearance of cerebrospinal fluid fistulas and the development of possible infectious complications.
Diagram of cranialization of frontal sinus.
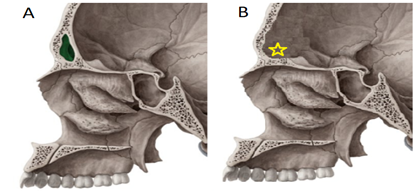
Figure 4: Diagram illustrating cranialization in frontal sinus fractures involving the posterior wall (with extensive destruction of the posterior wall or CSF fistula. In image A the frontal sinus can be seen in green. Image B shows the cranialization of the frontal sinus (yellow star).
Linear fracture without cerebrospinal fluid fistula
Displaced or comminuted fracture with cerebrospinal fluid fistula
Cerebrospinal fluid (CSF) is the fluid that surrounds the brain and spinal cord. When this fluid leaks through the nose it is usually the result of a cerebrospinal fluid fistula, which occurs when there is a rupture or tear in the membranes that contain it. There are some ways to identify it [7]:
One of the most commonly used approaches is the bicoronal approach, although the approach through the facial wounds in case they exist may be an alternative to consider. In very particular cases an upper blepharoplasty incision can be performed. Fixation after reduction in most cases is performed with low profile titanium mini-plates [4].
Currently, for the treatment of fractures of the anterior wall of the frontal sinus, the bicoronal approach can be replaced in certain cases by the endoscopic approach, since it can reduce the surgical time, as well as reduce the aggressiveness of the intervention and improve the postoperative period [12-14].
Accurate clinical radiological diagnosis is essential to determine the appropriate treatment, as well as long-term follow-up, since complications may appear late. Reduction and osteosynthesis of posterior wall fractures, completed if necessary with obliteration of the nasofrontal canal and sinus, is a valid alternative to cranialization. It is therefore essential that the patient be evaluated and managed by a multidisciplinary team, which should include Maxillofacial Surgery, Otolaryngology and Neurosurgery.
Copyright: © 2024 Nicolás Ibáñez-Ballesteros.,et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.