Mendoza-Tapia Juan Pablo1*, Passalacqua-Molina Gianfranco2 and Villalobos-Chamorro Fernanda3
1Oral and Maxillofacial Emergency Resident, Clínica Alemana Santiago, Oral and
Maxillofacial Service, Faculty of Medicine - Universidad del Desarrollo, Santiago, Chile
2Maxillofacial Surgeon, Clínica Alemana Santiago Oral and Maxillofacial Service, Santiago,
Chile
3Oral and Maxillofacial Surgery and Traumatology Resident, Clinica Alemana Santiago, Oral
and Maxillofacial Service, Faculty of Medicine – Universidad del Desarrollo, Santiago, Chile
*Corresponding Author: Mendoza-Tapia Juan Pablo, Oral and Maxillofacial Emergency Resident, Clínica Alemana Santiago, Oral and Maxillofacial Service, Faculty of Medicine - Universidad del Desarrollo, Santiago, Chile.
Received: September 02, 2024; Published: September 18, 2024
Citation: Mendoza-Tapia Juan Pablo., et al. “Necrotizing Sialometaplasia: Diagnostic Challenges in a Case". Acta Scientific Dental Sciences 8.10 (2024):36-40.
Necrotizing sialometaplasia (SMN) is a rare benign pathology that mainly affects minor salivary glands. Its clinical presentations are associated with metaplastic processes of acinar cells, being a pathology confusing with neoplastic pathologies such as mucoepidermoid carcinoma. The latter can lead to erroneous diagnoses and unnecessary surgical interventions.
A 37-year-old woman presented to Clinica Alemana Emergency Service in Santiago due to probable symptoms of trigeminal neuralgia within 12 hours of evolution. The condition presents with paroxysmal hemifacial and palate pain accompanied by a burning sensation and numbness of the palate with no history. of trauma or stimuli to the painful areas. Through an exhaustive neurological examination, migraine symptoms or trigeminal neuralgia were ruled out. The intraoral examination revealed a discrete increase in volume associated with erythema in the hard palate area, referred to as a pain point by the patient. A magnetic resonance imaging was requested showing hypointense structures on T1, hyperintense T2, and a defined contour on the roof of the palate. Given the clinical and imaging characteristics, the diagnostic hypothesis of non-ulcerated necrotizing sialometaplasia is established, confirming its diagnosis by means of incisional biopsy.
Keywords: Necrotizing Sialometaplasia, Benign glandular pathology, Minor salivary glands
The hard palate is lined with masticatory-type mucosa that adheres firmly to the deep planes and exhibits dense connective tissue containing numerous collagen fibers, including scarce adipose tissue and multiple minor salivary glands [1]. The latter may present pathological structural changes, mainly of inflammatory or neoplastic origin. Among these pathologies, necrotizing sialometaplasia (NMS) is a benign self-limiting lesion triggered mainly by ischemic events produced by local trauma [2]. However, other less frequent triggers such as drug abuse and eating disorders such as bulimia are also described. These triggers, along with predisposing factors, such as the use of irritants such as alcohol, tobacco, and certain condiments, contribute to their appearance [3,4].
The clinical manifestations of NMS are characterized by both ulcerative and non-ulcerative manifestations associated with local and radiating pain. Both presentations are mainly located on the hard palate in the vicinity of the boundary with the soft palate. However, the ulcerative form is considered the classic presentation which can be confused with neoplastic lesions [4]. Nonulcerative presentation is less common and presents with subtle changes such as slight increases in volume associated with surrounding erythema.
The diagnosis is made based on its histological characteristics, where areas of necrosis and metaplasia are present, preserving the salivary lobular architecture. This last characteristic stands out as a desirable diagnostic criterion. However, lobular preservation may be lost, and duct and acinar metaplasia may mimic the histological image of mucoepidermoid carcinoma [2].
Due to its clinical manifestations and the metaplastic processes produced by this pathology, it can lead to misdiagnosis and unnecessary surgical interventions compromising surrounding tissues.
This case report was carried out with the aim of describing the diagnostic process and management of a diagnosed NMS in a 37-year-old patient treated in the Maxillofacial Service of Clínica Alemana de Santiago in 2023.
A 37-year-old female patient consulted the Emergency Department of the German Clinic in Santiago for probable trigeminal neuralgia, reporting acute pain (10/10 VAS) within 12 hours of evolution. Within the patient's medical history, she mentions being treated for Hashimoto's thyroiditis, dyshidrosis, insulin resistance, mood disorder and bulimia. No history of allergies, smoker of 5 cigarettes a day.
In anamnesis, the patient reported 7 days ago having had viral respiratory symptoms, which is accompanied by hemifacial and palate pain crises during the last 3 days. In the last 12 hours, she presented paroxysmal facial pain VAS 10/10 accompanied by photophobia, sonophobia and epiphora. In addition, he reports a burning sensation and numbness of the palate. It does not mention any type of trauma or stimulus associated with the area where the pain is reported.
Initial symptomatic management was performed in the emergency service with ketorolac 30 mg/ml injection, paracetamol 1000 mg/100 ml intravenously (EV), dexamethasone 4 mg/ml injection, phenytoin 500 mg/250 cc EV and fentanyl 30 mcg. Neurological examination ruled out migraine or trigeminal neuralgia. Intraoral examination showed erythema on the boundary between the hard and soft palate and a slight increase in volume on the left side of the hard palate with a soft consistency and a smooth surface (Figure 1), painful to palpation (VAS 10/10). Magnetic resonance imaging was requested, which showed hypointense structures in T1, hyperintense T2 and a defined contour on the roof of the palate bilaterally, approximately 16 x 6 mm (Figure 2). Based on the clinical and imaging characteristics, the diagnostic hypothesis of non-ulcerated necrotizing sialometaplasia is established. Despite being a self-limiting benign pathology with spontaneous resolution, the patient requested an incisional biopsy to confirm this diagnosis, which was performed with 5mm PUNCH under local anesthesia (Figure 3A-3B).
In the histopathological analysis of the sample, acini of the minor salivary gland with preservation of architecture and with extensive associated necrosis are recognized, the acinar cells present pycnotic nuclei with effacement of the cell boundaries and extravasation of mucin, associated with cellular detritus (Figure 4). The above findings confirm the diagnosis of necrotizing sialometaplasia. Symptomatic management was carried out along with indication of local and general care.

Figure 1: Increased soft volume in the hard palate on the left side close to the border with the soft palate.
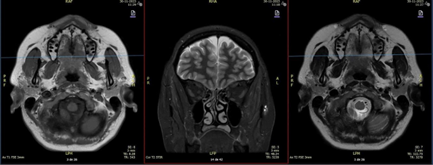
Figure 2: The report describing the MRI mentions Tl hypointense, T2 hyperintense, defined contour, cystic-looking structures on the roof of the palate bilaterally, approximately 16 x 6 mm, non-specific.

Figure 3: A) Obtaining biopsy with 5mm Tissue PUNCH. B) Surgical biopsy site.
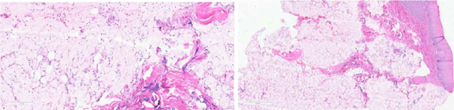
Figure 4: Histological sections. Minor salivary gland acini with conservation of architecture and with extensive associated necrosis, the acinar cells present pyknotic nuclei with effacement of cell boundaries and extravasation of mucin, associated with cellular debris.
At the 5-day check-up of the biopsy, the patient reported notable relief of the painful symptoms. Intraoral examination showed extension of the biopsy bed margins with surrounding tissue with normal clinical features. Within the bed, self-limiting necrotic tissue is observed, expected in the context of diagnosis (Figure 5).

Figure 5: 5-day post-biopsy control. Extension of biopsy bed margins with surrounding tissue with normal clinical characteristics. Self-limiting necrotic tissue is observed within the bed.
At the 14-day check-up, the patient was asymptomatic. Intraoral examination shows that the margins of the surgical bed have been maintained since the last control. Necrotic tissue was carefully removed (Figure 6A) and local cleaning was performed with saline solution in the area, favoring the observation of the fundus of the bed, which presents a fibrin lining compatible with the normal healing process (Figure 6B).
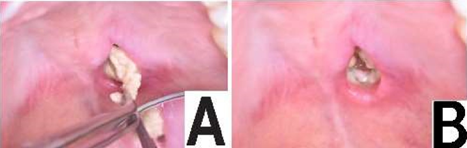
Figure 6: A - B. 2-week post-biopsy control. A) The presence of solid yellowish-white tissue compatible with necrotic tissue is observed in the biopsied area. B) The bottom of the biopsied area is observed covered by a layer of fibrin compatible with a normal healing process.
To carry out this report, the patient read and signed the informed consent prepared for this report.
NMS is a benign inflammatory lesion that affects the minor salivary glands of the mucosa of the palate and represents a small number of all biopsied lesions of the oral cavity [5], being considered a rare pathology. Knowledge regarding its etiology and pathophysiology is limited. It is postulated that it is caused by ischemia of the salivary glands induced mainly by trauma or ischemic agents such as those produced when applying local anesthetic with vasoconstrictor that includes both. However, chronic irritants such as acids produced by diet, gastrointestinal reflux or eating disorders as well as alcohol are also postulated [5,6]. In our reported case, there is no history of previous trauma, however, the patient has an eating disorder that exposes the tissues of the oral cavity to acids on a recurrent basis that, together with the daily consumption of tobacco, can generate avascularity and inflammation of the tissues, which can be attributed to these factors as triggers of the pathology [3,4]. In terms of its location, SMN can occur in other sites such as the lower lip, jugal mucosa or tongue, all of which are less frequent than its presentation on the palate [7]. When they appear in the latter, they occur more frequently unilaterally (88.9%) than bilaterally (2.8%) [2]. The SMN.
In addition, it can present in an ulcerated and non-ulcerated form, both accompanied by painful symptoms [4]. In our report, although it occurs in the most frequent location on the palate and unilaterally, the non-ulcerated presentation is the least frequent, accounting for a third of the cases of NMS [7]. In some articles, the non-ulcerated form is proposed as a step prior to ulceration, in others the surface of the tissues remains unharmed and it is suggested, given a clinical certainty of this pathology, not to perform interventions such as biopsy as it could generate a greater comorbidity of the site. However, biopsy is essential for definitive diagnosis.
Differential diagnoses are established according to each of these presentations. In the non-ulcerated form, a normal tissue appearance is observed, they may present as an increase in firm volume, erythema and surrounding inflammation, which could indicate a possible pleomorphic adenoma, this being the most common benign tumor of the salivary glands [8,9]. In its ulcerated form, the clinical features of mucoepidermoid carcinoma are the most common malignant tumor of the salivary glands [4]. Histopathology, based on their histological characteristics, will allow us to differentiate these pathologies. In NMS, the absence of myoepithelial cells and the presence of areas of necrosis and metaplasia rule out pleomorphic adenoma. In addition, the salivary lobular architecture is preserved in the NMS. However, in rare cases, lobular preservation may be lost and metaplasia of ducts and acini may mimic the histological image of mucoepidermoid carcinoma, making this a diagnostic challenge for the pathologist [11,12]. In our case, the histopathological analysis showed minor salivary gland acini with preservation of the architecture and with extensive associated necrosis, allowing the accurate diagnosis of the pathology.
Management involved educating the patient about this benign, self-limiting pathology with spontaneous resolution in approximately 2 to 3 months [10,13,14]. Symptomatic pharmacological treatment and outpatient controls were maintained for correct healing and the absence of comorbidities.
Necrotizing sialometaplasia (NMS) is a rare benign pathology that mainly affects minor salivary glands, its clinical presentations are associated with metaplastic processes of acinar cells, being a pathology confused with neoplastic pathologies such as mucoepidermoid carcinoma. The latter can lead to misdiagnosis and unnecessary surgical interventions.
A 37-year-old woman presented to the Emergency Department of the German Clinic in Santiago for probable trigeminal neuralgia with 12 hours of evolution, the condition presented with paroxysmal hemifacial and palate pain accompanied by burning sensation and numbness of the palate without a history of trauma or stimuli to the areas of pain. A thorough neurological examination ruled out migraine or trigeminal neuralgia. Intraoral examination showed a discrete increase in volume associated with erythema in the hard palate area, referred to as the pain point by the patient. Magnetic resonance imaging was requested where hypointense structures in T1, hyperintense T2 and defined contour in the roof of the palate were observed. Based on the clinical and imaging characteristics, the diagnostic hypothesis of non-ulcerated necrotizing sialometaplasia is established, confirming its diagnosis by incisional biopsy.
Necrotizing sialometaplasia is a rare pathology that is difficult to diagnose, with non-ulcerated NMS being a rare presentation and scarcely documented in the literature.
Copyright: © 2024 Mendoza-Tapia Juan Pablo., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.