Hala Abdullatif1*, Nayer Aboelsaad2, Khaled Abed El Galil3
1MS in Periodontology, Faculty of Dentistry, Beirut Arab University, Lebanon
2Associate Professor of Periodontology, Faculty of Dentistry, Beirut Arab University, Lebanon
3Associate Professor of Pharmaceutical Sciences, Faculty of Pharmacy, Beirut Arab University, Lebanon
*Corresponding Author: Hala Abdullatif, MS in Periodontology, Faculty of Dentistry, Beirut Arab University, Lebanon.
Received: October 29, 2018; Published: December 04, 2018
Citation: Hala Abdullatif., et al. “Management of Gingival Hyperplasia in Patients with Fixed Orthodontic Appliances Using Topical Herbal Preparations (A Comparative Clinical and Microbiological Study) ”. Acta Scientific Dental Sciences 3.1 (2019): 02-11.
Purpose: The purpose of this study was to compare the effectiveness of Acacia Arabica (AA) and Tea Tree Oil (TTO) gels in the treatment of gingival inflammation and enlargement in patients with fixed orthodontic appliances.
Materials and Methods: Three groups of 30 patients under orthodontic treatment having gingival enlargement were selected randomly with age range from 18 - 30 years old and divided into 10 patients in each group. Where patients in Group A treated with scaling and root planing (S/RP) in addition to the application of Acacia arabica gel. Patients in Group B were treated with S/RP and application of TTO gel, whereas patients in Group C were treated with S/RP alone. The presence of supragingival biofilm and marginal gingival bleeding were recorded with the PI (Plaque index), GI (Gingival index), BI (bleeding index), PD (probing pocket depth) and GOG (gingival overgrowth index). Subgingival plaque was collected using sterilized Gracey curette by inserting it subgingivally into the deepest portion of the periodontal pocket, and then samples were evaluated using multiplex PCR after DNA extraction.
Each participant had been clinically evaluated at baseline (T0), after 1 month (T1) and after 3 months (T2). Plaque samples were collected from each participant at T0 and at T2.
Results: Acacia arabica gel showed significant clinical improvement (P < 0.05) at the end of the study with a mean value score of plaque index (0.9) in group A as compared to control group C (1.8). This improvement was comparable to Tebodont gel (0.9) in group B. These results were almost the same for GI, BI, PD and GOG index. Also bacterial count showed a reduction from baseline and after 3 months with significant difference in group A and B comparing them with group C. P. gingivalis bacteria was detected, with reduction in its count. The difference between the two herbal gels with regard to clinical and microbiological parameters were not found to be significant at any time interval.
Conclusion: The two different polyherbal gels can be used as an adjunct measure to scaling and root planning and other plaque control methods to treat or reduce clinical and microbiological signs of gingivitis and gingival enlargement in patients with fixed orthodontic appliances.
Keywords: Gingival Overgrowth; Orthodontic Patients; Acacia Arabica Gel; Tea Tree Oil Gel
It is known that orthodontic appliances could compromise the maintenance of optimum oral hygiene even in the most meticulous patient. Although in most children undergoing orthodontic therapy, with no previous history of loss of attachment or periodontal disease, the only consequence of wearing orthodontic appliances is a transient gingivitis caused by dental plaque. After completion of orthodontic therapy, this problem usually resolves because of ease in the access of inter-dental cleansing [1].
Adequate levels of plaque control are difficult to achieve in patients with fixed orthodontic appliances. As a result, orthodontic patients often develop gingivitis, with the response characterized by gingival inflammation and hyperplasia. So It is important to have good dental hygiene during your orthodontic treatment to avoid gum swelling. Powered tooth brushes and various chemical agents have been shown as beneficial adjuncts to normal manual tooth brushing for plaque removal in orthodontic patients [2].
The use of antimicrobial mouthwashes as an adjunct to mechanical oral hygiene has become well established in dental practice for the control of supra-gingival plaque and gingivitis. A broad variety of antiseptic mouthwashes is offered for patient selection. Chlorhexidine (CHX), a bisbiguanide, considered to date the most effective antiplaque agent, is not easily formulated into toothpastes, and local side effects, especially reversible brown staining of teeth, tongue and resin restorations, and transient impairment of taste perception have limited the long term use of CHX as a mouthwash. The problem associated with side effects stimulated the search for alternative antiplaque, antigingivitis agents [3].
Mechanical debridement has been the most widely used approach, but many studies have shown that mechanical debridement alone cannot effectively eliminate most of the causative bacteria and it is usually associated with high recurrence rate. Unwanted side effects such as resistance, toxicity, sensitivity, growth of opportunistic infection and interaction with other medications are often encountered [4].
Natural products have served as a major source of drugs for centuries and about half of pharmaceuticals in use today are derived from natural products. Oriental medicines have been evaluated for their effects on periodontal disease, regarding the antibacterial and anti‑inflammatory effects as well as the periodontal tissue regeneration.
Among these materials that have an anti-plaque agent and can be used on a daily basis with minimal side effects [5].
Acacia Arabica gel, is one such polyherbal formulation with Acacia arabica as its main Acacia gum consists primarily of Arabica, a complex mixture of calcium, magnesium and potassium salts of Arabic acid [6]. It contains tannins which are reported to exhibit astringent, haemostatic and healing properties. It also contains cyanogenic glycosides in addition to several enzymes such as oxidases, peroxidases and pectinases, all of which have been shown to exhibit antimicrobial properties [7].
The short-term clinical effects of a commercially available prescription gel containing Acacia arabica in the reduction of plaque and gingival inflammation in subjects with gingivitis were assessed and it was found that its efficacy is comparable to chlorhexidine. Apart from this, Acacia arabica gel can be used for an extended period of time unlike chlorhexidine which causes tooth discoloration and has an unpleasant taste [8].
Tea Tree Oil gel is mainly composed of 2% tea tree oil, tea tree oil (TTO) is derived from the paper bark tea tree. Tea tree oil is an essential oil obtained by steam distillation of the leaves of Melaleuca alternifolia, a plant native to Australia.
Historically, the leaves were used as a substitute for tea, which is how tea tree oil got its name. The part used medicinally is the oil from the leaves. TTO has a broad-spectrum antimicrobial, antifungal, antiviral, antioxidant and anti‑inflammatory effect. These activities were shown to be related to the active ingredients such as 1,8-cineole and terpinen-4-ol [9].
The null hypothesis: no difference between the application of Tea Tree Oil gel as well as Acacia Arabica gel in reducing the gingival overgrowth in patients with fixed orthodontic appliances.
Thirty participants with fixed orthodontic appliances having gingival hyperplasia will be selected and meeting the following criteria.
All Participants should have:
Each subject was chosen at random to enter one of the treatment groups using random number. The treatment group was randomly divided into three groups:
Scaling and root planing was performed for all the groups scheduled at baseline (T0), after one month (T1) and three months (T2).
A full-mouth periodontal examination was performed. The presence of supragingival biofilm and marginal gingival bleeding were recorded with the Gingival index (GI), Bleeding on probing, (sulcus bleeding index),
PD, (periodontal depth) BI (bleeding index), and GOG (gingival overgrowth index). After this subgingival plaque was collected using sterilized Gracey curette and then transported using Sodium Thioglycolate medium for microbiological analysis.
All of the patients were instructed, and shown how to apply a pea-sized amount of gel to their gingiva twice a day, immediately after brushing. The gel was applied to their buccal and lingual/ palatal gingiva. They were then instructed to thoroughly expectorate, and to avoid rinsing, eating or drinking for at least 30 minutes. Patients were instructed to continue this regimen twice a day for 1 month with instructions for oral hygiene maintenance.
Detailed clinical history will be recorded and clinical assessments will be carried out for all participants. Subgingival plaque samples will be collected, subjected to DNA extraction and subsequent PCR for detection of different microbes. Participants in 3 groups will be evaluated for clinical parameters and microbiologically for the presence of periodontal microbes.
Each participant will be clinically evaluated at baseline (T0), after 1 month (T1) and after 3 months (T2). And the following clinical parameters will be measured and recorded:
The subgingival plaque is further processed in the lab as follows. From the thioglycolate broth, sub cultures are made on blood agar and incubated aerobically as well as anaerobically. Pre reduced Sheep blood agar plates are used for anaerobic culture. The inoculated plates are incubated for 72 hours, and examined for the growth of aerobic and anaerobic bacteria. Colony counting was done by visual counting on number of colonies using colony counter score of Vajawat where [10]:
Bacterial identity was confirmed using multiplex PCR. For DNA extraction, the collected samples in PBS buffer were thawed, vortexmixed for 1 minute, and then centrifuged at 5000 rpm for 5 minutes. The initial volume of 500 µL was then reduced to 300 µL to increase the concentration of microbial cells. Samples are boiled in water bath for 10 min, and then frozen at -20ºC for further analysis. Reference DNA for the microorganisms under analysis (example, S. mutans ‑ ATCC 25175, P. gingivalis - ATCC 33277 and P. intermedia - ATCC 25611) were also extracted to serve as positive controls.
Joshi., et al. (2010) disused the steps in PCR, There are three major steps involved in the PCR technique: denaturation, annealing, and extension.
PCR products were analyzed by running gel electrophoresis in 1.5% agarose (w/v) in Tris‑ borate‑EDTA buffer stained with ethidium bromide then illuminated under U.V transilluminator. In the meantime,100 bp DNA ladder was used as DNA size marker.
Analysis of data was carried out using SPSS 23.0 (SPSS, Chicago, IL, USA). The values of different parameters collected are expressed as means + standard Deviation (SD). Normality of continuous data was tested using Chi test and t-test. Mean score change from baseline, after 1 month and 3 months were calculated. Comparison between the three treatment groups and within each treatment group was performed using one-way analysis of variance (ANOVA). Statistics were significant at the 0.05 level.
All the patients completed the study without any complications. At baseline, there was no significant difference with respect to any clinical parameter between the groups.
Table 1 shows that at T0 there was no significant difference in the results between all groups A significant reduction in the mean score of the PI was observed from baseline T0 till T1 in the 3 groups with slight difference, where the reduction in group A and group B was almost the same where as in group C the reduction was less than the other groups. Then the reduction of the mean score from T1 till T2 was not significant in all groups as well. From T1 till T2 was not significant in all groups as well these results are illustrated in table below.
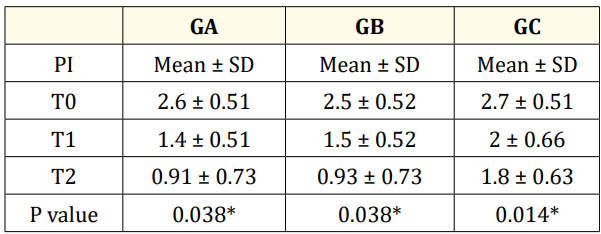
Table 1: Mean values, standard deviation and P value
of PI among the study groups at T0, T1 and T2.
*: Statistically significant at p ≤ 0.05.
Table 2 shows that the gingival index from T0 till T1 was reduced significantly (from 2.6, 1.6 respectively) in group A with no significant difference with group B (from 2.4, 1.5 respectively) with P = 0.7 between the two groups at T1. Where in group C the reduction was not significant as in group A and B. (from 2.7, 2 respectively) where (P = 0.01 for group A compared with group C) and (P = 0.006 when group B compared with group C). From T1 till T2 the reduction in the mean score of GI in the 3 groups was not significant but the reduction in group A and B was much more that in group C.
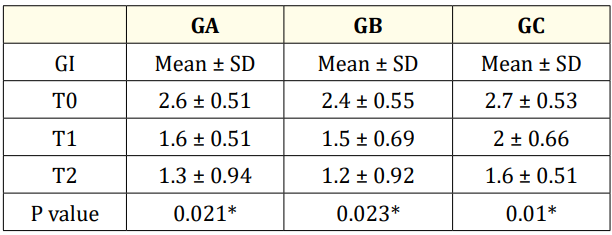
Table 2: Mean values, standard deviation and p value of
GI among the study groups at T0, T1 and T2.
*: Statistically significant at p ≤ 0.05.
Table 3 shows the mean score of BI which was significantly reduced from baseline T0 till T1 in the 3 groups, but both groups A and B showed more significant reduction when compared with group C. for group A (4.5, 1.6 respectively), (4.4, 1.5 respectively) for group B and (4.3, 3 respectively) for group C. From T1 till T2 the reduction in the mean score of BI in the 3 groups were not significant, but both group A and B showed more reduction in the BI score than group C.
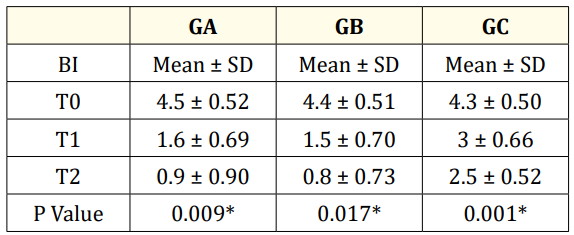
Table 3: Mean values, standard deviation and P value
of BI among the study groups at T0, T1 and T2.
*: Statistically significant at p ≤ 0.05.
Table 4 shows a high reduction in the mean score of the PD in all groups but with no significant difference between group A and B (P = 0.7) while it shows a significant difference between these two groups and group C respectively (P = 0.01, P = 0.006). At T2 there was no a significant difference in the reduction of PD score among the 3 groups, but both groups A and B showed a reduction in PD better than in group C. The mean score of PD at T2 for group A was 1.2, group B 1.3 and in group C 2.2.
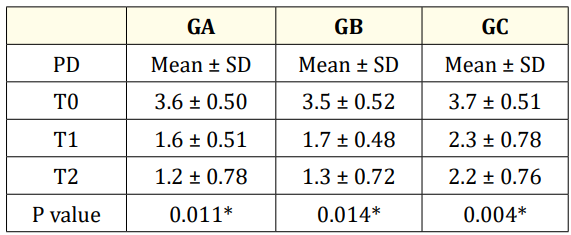
Table 4: Mean values, standard deviation and p value
of PD among the study groups at T0, T1 and T2.
*: Statistically significant at P ≤ 0.05.
Table 5 shows that the mean score of GOG index was reduced from T0, T1 till T2, (3.3, 1.5 and 1.1 respectively) in group A, in group B (3.5, 1.6 and 1.2 respectively) and in group C (3.6, 3, and 2.5 respectively), the reduction was significant among all groups from T0 till T1 with no significant difference between group A and B while a significant difference was present when comparing group A and B with group C. At T2 the reduction was less significant in the 3 groups as the reduction in T1 with no significant difference between group A and B.
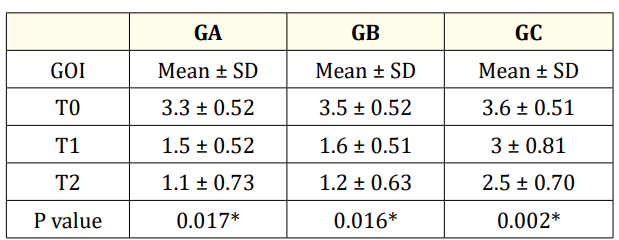
Table 5: Mean values, standard deviation and P value
of GOI among the study groups at T0, T1 and T2.
*: Statistically significant at P ≤ 0.05.
For Microbiology results, all plaque samples had been taken from the buccal site of the lower anterior teeth were analyzed in each patient in the 3 groups at 2 different time points T0 and T2 (where T0 is the time of collection before the tested herb and T2 is 3 months after treatment). Table 6 shows the percentage of the average mean of the bacterial count between the three groups A, B and C at baseline T0 and after 3 months T2. There was a gradual reduction in the score of the bacterial count among the three groups from T0 till the end of the study T2 but with no statistical significant difference where all the samples colony counter score was 4+ as the count exceeded 100,000 CFU/µl.
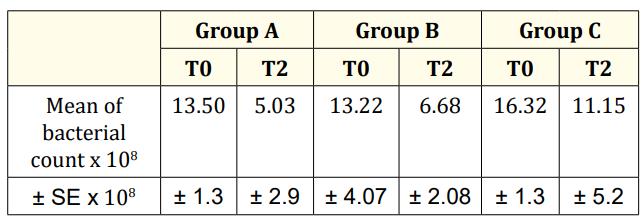
Table 6: Mean value for bacteria count at T0 and T2 for 3 groups A, B and C.
Gram staining and the microscopic examination of the collected surface colonies have shown that the isolated microorganisms were Gram negative rods and Gram positive cocci as seen in figures 1 below.
The isolated bacteria from the plaque did not show any characteristic findings and PCR was the main way for defining the type of bacteria found in the collected samples.
The target of this study was to identify the prevalence of three periodontopathic bacteria (Tannerella forsythia, Porphyromonas gingivalis, Treponema denticola).
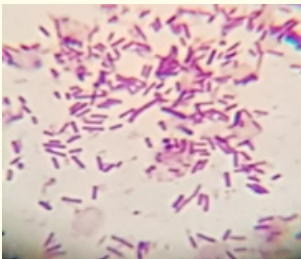
Figure 1: Gram negative rods.
In order to identify the presence of the target anaerobic bacteria, multiplex PCR was performed. Ubiquitous primer has shown the presence of such bacteria in most of the isolated plaque samples as seen in figure 2 below.
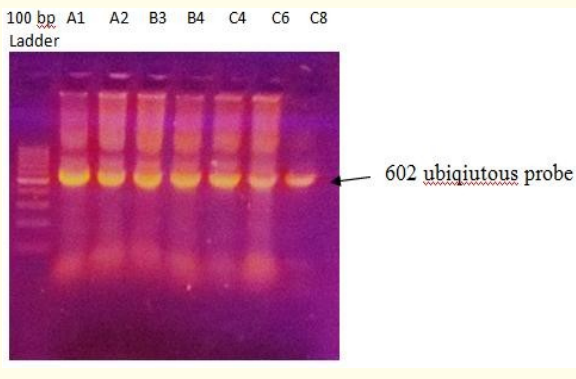
Figure 2: Gel electrophoresis of PCR amplification of anaerobic bacteria using ubiquitous primer (602 bp).
The molecular analysis of the samples treated by A or B and untreated C have shown the presence of Porphyromonas gingivalis at parentages 70%, 60%, and 80%, respectively at T0. After T2, the detection level of Porphyromonas gingivalis has reached 40%, 40%, and 70%, respectively for the same samples.
Microbiological results for sub-gingival plaque samples in the present study only Porphyromonas gingivalis (Pg) had been detected using PCR and gel electrophoresis (Figure 2) with no detection of other bacteria that were under study. Porphyromonas gingivalis bacteria had been detected at T0 and T2, with no significant reduction in the bacterial count in each group of the study, but the difference between group A and B was not significant but it was significant when it is compared with group C (Table 7 and Figure 3).
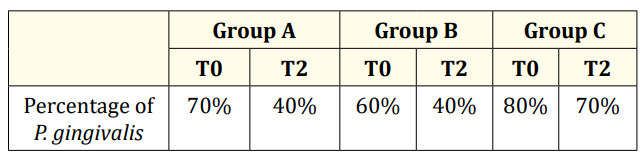
Table 7: Percentage of P. gingivalis in the 3 groups at T0 and T2.
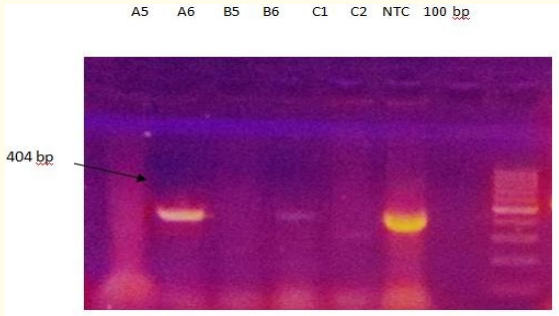
Figure 3: Gel electrophoresis of PCR amplicon (404 bp) for the detection of Porphyromonas gingivalis using PCR specific primers. Lanes (2, 4, and 6). Lane 7 as a negative control.
Patient in Group A before treatment procedure (Acacia Arabica + S/RP).

Figure 4: Patient with Gingival Hyperplasia at T0 of gingival enlargement of grade 3.

Figure 5: Patient with Gingival Hyperplasia at T1 of gingival enlargement of grade 1.
Patient in Group B before treatment procedure (Tea Tree Oil + S/RP).

Figure 6: Patient with gingival hyperplasia at T0 of gingival enlargement of grade 3.

Figure 7: Patient with Gingival Hyperplasia at T1 of gingival enlargement of grade 1.
The purpose of this study was to determine the clinical and microbiologic effects of polyherbal gel containing Acacia arabica on plaque and gingival inflammation in subjects with gingivitis caused by orthodontic treatment and to compare these effects to Tea Tree Oil gel. Both the Acacia arabica gel and TTO gel groups showed significant improvement in the clinical parameter scores at all time intervals. Microbial counts were significantly reduced from baseline to 3 months and the results were comparable to a control group which treated only with S/RP.
The study done by Zanatta., et al. [11] was aimed at investigating potential associations among gingival enlargement, sociodemographic and clinical characteristics and the results of the mean value for anterior gingival enlargement GE, percentage of whole mouth visible plaque PI and percentage of whole mouth visible plaque PI and percentage of whole mouth gingival bleeding BI were 0.69, 47.38% and 58.72%, respectively.
Gorbunkova., et al. [12] discussed the impact of orthodontic treatment on periodontal tissues, and reported during OTM some adverse effects on the soft periodontal tissue may be observed. The most frequently occurring changes in soft tissues are gingival overgrowth (GO), gingival recessions (GR), and gingival invaginations (GIs), which commonly occur in orthodontic extraction cases.
Microbiological studies by Paolantonio., et al. [13] demonstrate that when fixed orthodontic appliances are placed, the potential for quantitative and qualitative changes in the microbial composition of these areas enhances. Thus, periodontal reaction might be elicited by a change in the microbiological environment.
In our study the microbiological analysis was focused on different oral bacterias where their prevalence may increases due to gingival inflammation and periodontal disease in patients with orthodontic treatment, as the study done Brett., et al. [14] who examined the periodontal and microbiological status of patients undergoing orthodontic therapy. The three periodontal pathogens that are known to inhabit the plaque and contribute to periodontal disease are Porphyromonas gingivalis, Treponema denticola and Tannerella forsythia. These bacteria are anaerobic periodontal pathogens capable of initiating periodontal destruction.
Pradeep [15] several studies have suggested that herbal products such as tea tree oil and Acacia Arabica gels inhibit periodontal pathogens and the destruction of the periodontal tissue.
In this study, we examined a gel containing Acacia arabica to evaluate its effects on periodontal health using a randomized, study design.
In the present study, the application of Acacia arabica-containing gel showed considerable reductions in plaque accumulation and gingival inflammation. Reductions in the PI showed in table 1. The reduction in PI scores may be due to the antimicrobial property of Acacia arabica, which is supported by Tambekar., et al [16].
GI scores recorded were also showed a reduction for the test group A during the study in comparison with GI at the baseline. These results were in accordance with a study of Pradeep., et al. (2010), where in his study the reduction in GI scores by Acacia Arabica gel was significantly higher than the placebo group and similar to the CHX gel group.
In the present study, a significant reduction in BI was observed in the test group A using the Acacia arabica gel in comparison with the control group C. These results were in line with the findings of Rameshwari., et al [17].
The GOG index in this study at group A showed a significant reduction from baseline till end of the study. These results gave the Acacia Arabica gel an advantage over S/RP alone in the reduction of gingival overgrowth, where in the study done by Draghici., et al. [18], she discussed the local causes of gingival over growth and concluded that gingivitis is reversible after scaling and root planning in initial stages combined with correct oral hygiene.
In this study the prevalence of bacteria in group A with Acacia arabica gel during study period was significantly lower than their prevalence in the control group C and this was coordinated with an in vitro study by Clark., et al. [19] revealed protease activity inhibition in the presence of 0.5% w/v of Acacia A gum.
However, our results showed that there was a statistically significant reduction in the mean PI scores during the study periods in both groups B and C as compared with baseline values and there was a significant difference between the two groups during the study periods. TTO also results in less plaque formation as reported by Shaila., et al. [20] who concluded that TTO could account for the antiplaque and antigingivitis activities of the formulated mouthrinse.
It was apparent in the present study that Group B (TTO gel + SR/P) showed a statistically significant reduction in gingival inflammation GI, which was maintained until the end of the study period as compared with Group C (SR/P only). This could be attributed to the anti‑inflammatory and antibacterial effect of the TTO. Cox., et al. [21] showed that the antimicrobial action of TTO results from its ability to disrupt the permeability barrier of microbial membrane structures.
The results of this study showed significant reduction in score of BI in Group B when compared to baseline scores and control group. This was similar to the study of Soukoulis and Hirsch [22].
This study also aimed to demonstrate the efficacy of TTO gel based on essential oil in controlling the prevalence three bacterial organisms that could cause and expression of gingivitis and gingival enlargement. The count of microbial organisms showed a significant reduction from baseline T0 till T2 after (3 months) and the reduction was more in the group B when compared with the control group C. In group B there was a significant reduction in bacterial count and this was also proved by study done by Veenu., et al [23].
In spite of the limitations of our study, we can say that local application of Acacia Arabica and TTO gels may provide some beneficial therapeutic effects to augment the results of SRP.
From this study it could be concluded that strict oral hygiene instructions and frequent oral prophylaxis can reduce gingivitis and gingival enlargement in patients who are under fixed orthodontic treatment. Acacia arabica and TTO gels can be used as an adjunct measure as other plaque control methods.
Copyright: © 2019 Hala Abdullatif., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.