Biruck Gashawbeza* and Gelila Gashawbeza
Department of Clinical Case Report, Ethiopia
*Corresponding Author: Biruck Gashawbeza, Department of Clinical Case Report, Ethiopia.
Received: July 23, 2024; Published: September 20, 2024
Citation: Biruck Gashawbeza and Gelila Gashawbeza. “HPV Beyond Simple Genital Warts: HIV Associated Huge Genital Condyloma Acuminates Case Series Managed with Skinning Vulvectomy from Addis Ababa, Ethiopia, SPHMMC". Acta Scientific Clinical Case Reports 8.10 (2024):38-41.
Human papillomavirus (HPV) infection, a common sexually transmitted infection, can manifest in various ways, from asymptomatic infection to the development of genital warts. While most HPV infections resolve spontaneously, certain individuals, particularly those with compromised immune systems, may experience persistent or recurrent infections. This case series investigates the management of three patients with extensive vulvar condyloma accuminata, also known as Buschke-Löwenstein tumors, associated with HIV infection. All three cases were referred to the Surgical Department of the St. Paul's Hospital Millennium Medical College (SPHMMC) in Addis Ababa, Ethiopia for skinning vulvectomy, a surgical procedure used to remove the wart-like growths. The report highlights the complexity of managing these cases, the challenges encountered, and the surgical outcomes observed. The study emphasizes the importance of early detection and timely referral to specialists in managing HPV-related lesions, especially in patients with HIV co-infection.
Keywords: Human Papillomavirus (HPV); Ethiopia
Human papillomavirus (HPV) is a ubiquitous group of viruses, with numerous types causing a variety of clinical manifestations, including benign skin lesions, cervical cancer, and vulvar cancer. HPV infection is the most common sexually transmitted infection among young adults. While most individuals infected with HPV are asymptomatic and clear the virus, certain individuals develop clinical manifestations such as genital warts [1,2]. These lesions, commonly referred to as condyloma acuminata, are usually small and amenable to local ablative treatments such as topical medications, cryotherapy, or laser therapy. However, in some cases, particularly in individuals with compromised immune systems, the infection can become persistent and lead to the development of large, invasive lesions known as Buschke-Löwenstein tumors [3]. These tumors can be locally aggressive, infiltrating surrounding tissues and causing significant morbidity. The presence of HIV co-infection is a major risk factor for the development of these aggressive HPV-related lesions. HIV infection compromises the immune system, making it difficult for the body to effectively clear HPV. This can lead to the uncontrolled growth of HPV-infected cells, resulting in the formation of large, invasive tumors. This case series presents the management of three patients with extensive vulvar condyloma acuminata in the context of HIV infection [4]. These cases highlight the challenges associated with managing these complex lesions and underscore the importance of early detection and timely referral for appropriate management.
This retrospective case series was conducted at the St. Paul's Hospital Millennium Medical College (SPHMMC), a tertiary care teaching hospital in Addis Ababa, Ethiopia. The study included three patients diagnosed with giant vulvar condyloma acuminata who were referred to the Gynecologic Oncology Department for surgical management. All patients were HIV positive and receiving anti-retroviral therapy (HAART). The patients' medical records were reviewed to obtain demographic information, clinical presentation, laboratory findings, and treatment details. The primary outcome measured was the success of the surgical procedure, defined as complete removal of the vulvar condyloma accuminata without recurrence. The patients' medical records were reviewed retrospectively. Data collected included demographic characteristics, clinical presentation, laboratory findings, HIV status, CD4 count, and treatment details. The primary outcome measure was the success of the surgical procedure, defined as complete removal of the vulvar condyloma accuminata without recurrence.
A 35-year-old woman presented with a massive vulvar lesion obstructing her vaginal opening. The lesion had been present for several years and was progressively growing. The patient reported significant discomfort, pain, and difficulty with ambulation. She was HIV-positive and on ART with a CD4 count of 350 cells/µL. She underwent skinning vulvectomy with no intra-operative complications. However, she developed a superficial wound infection post-operatively, which was successfully treated with local wound care. The patient experienced a significant improvement in her symptoms and quality of life.

Figure 1: Case 1 pre-surgery.
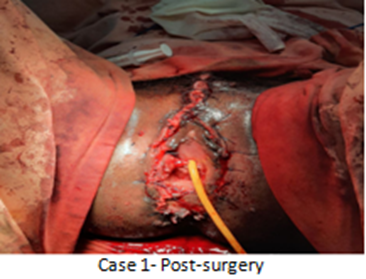
Figure 2: Case 1 posts –surgery.
A 42-year-old woman presented with a large, cauliflower-like vulvar lesion causing significant discomfort and pain. The lesion had been present for over a year and was progressively growing. She was HIV-positive and on ART with a CD4 count of 400 cells/ µL. She underwent skinning vulvectomy with no intra-operative complications. The patient reported improvement in her symptoms after the procedure. Follow-up examinations showed no signs of recurrence.

Figure 3: Case 2 Pre- surgery.
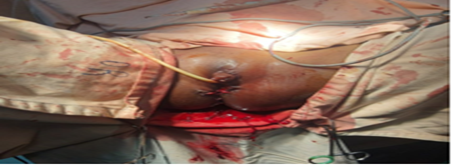
Figure 4: Case two post-surgery.
A 10-year-old girl presented with a large, pedunculated vulvar lesion that was obstructing her vaginal opening. The lesion had been present for several months and was progressively growing. She was HIV-positive and on ART with a CD4 count of 250 cells/µL. This case is notable for its occurrence in a pre-menarcheal girl, highlighting the potential for HPV-associated lesions to develop at an early age. She underwent skinning vulvectomy with no intra-operative complications. The patient experienced significant improvement in her symptoms and was able to engage in normal activities.

Figure 5: Case 3 Pre -surgery.

Figure 6: Case 3 post- surgery
Giant Vulvar condyloma accuminata, also known as Buschke-Löwenstein tumors, are a rare but challenging condition. These lesions can be locally aggressive and cause significant morbidity, particularly in patients with compromised immune systems. The presence of HIV co-infection is a major risk factor for the development of these aggressive HPV-related lesions [5]. Our case series highlights the challenges associated with managing these complex lesions, especially in patients with HIV infection. The delay in seeking treatment and referral can have a significant impact on the quality of life. The cases presented here highlight the importance of early detection and referral to specialists in managing HPV-related lesions, especially in patients
with HIV co-infection. Early referral to a gynecologic oncologist with experience in skinning vulvectomy can have a significant impact on the surgical outcome and quality of life [6]. The successful outcomes of skinning vulvectomy in these cases demonstrate its effectiveness in achieving complete resolution of giant vulvar condyloma accuminata lesions [7]. The successful outcomes of skinning vulvectomy in these cases demonstrate its effectiveness in achieving complete resolution of giant vulvar condyloma accuminata lesions [8]. This approach is particularly relevant for patients with HIV co-infection, where conventional local ablative treatments may be less effective [9].
The inclusion of a pre-menarchal girl in this case series emphasizes the importance of considering HPV-related lesions in young girls [10,11]. The challenges associated with managing these cases in young girls underscore the need for awareness among healthcare providers and the importance of prompt referral to specialists. Further research is needed to investigate the long-term outcomes of skinning vulvectomy in patients with HIV-associated giant vulvar condyloma accuminata. This research should include a larger sample size and a longer follow-up period to determine the rates of recurrence and other long-term complications.
The management of condyloma acuminata requires a comprehensive approach, taking into account the patient's individual needs and preferences. Treatment options range from topical therapies to surgical interventions and the choice of treatment will depend on the severity and extent of the warts, as well as the patient's medical history and overall health status. Regular follow-up is essential to monitor for recurrence and to ensure effective treatment.
HPV- Human papillomavirus, HIV- human immunodeficiency virus, SPHMMC -St. Paul's Hospital Millennium Medical College, HAART- highly active Antiretroviral therapy, CD4 -Clusters of differentiation- 4
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee.
Informed consent was obtained from all individual participants included in the study.
The paper and its supporting information files contain all necessary data.
BG served as the study's lead investigator, primary surgeon, collecting, entering, analyzing, and interpreting data, as well as preparing the report and acting as a corresponding author. GG contributed to the article's drafting or critical revision for essential intellectual content. The final document was read and approved by all authors, and they agreed to be responsible for all parts of the work.
Copyright: © 2024 Biruck Gashawbeza and Gelila Gashawbeza. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.