Kashyap Patel*, Asutosh Gor, Niyati Nathwani, Viral Rabara, Maharshi Patel, Ashima Kodali, Powers Thaddeus Norrell, Ola Jane Gulledge, Aashutosh Patel, Kaushal Patel, Shailesh Talati, Sandra Nixon, Shreya Nachane, Shreya Desai, Avni Kodali, Meggie Sullivan, Sandra Nixon, Benjamin Brown, Sara Rogers, Rohan Nadkarni, Carson Gallo, Danbey Asmer, Joseph Desimone, Devin Naidu and Sashi Naidu
Carolina Blood and Cancer Care, Rock Hill, SC, USA
*Corresponding Author: Kashyap Patel, Carolina Blood and Cancer Care, Rock Hill, SC, USA.
Received: August 26, 2024; Published: September 29, 2024
Citation: Kashyap Patel., et al. “A Treatment Journey to Remission, Multiple Recurrences, and Remissions: A Case Report of a Cholangiocarcinoma Patient Treated with Surgery, Adjuvant and Palliative Chemotherapy, Orthotopic Liver Transplantation, and SBRT Radiotherapy; A Journey from Despair to Hope Over a Decade”. Acta Scientific Cancer Biology 8.10 (2024): 14-16.
Cholangiocarcinoma (CCA) is a rare cancer associated with poor prognosis [1-3]. CCA is a cluster of highly heterogeneous biliary malignant tumors that can arise at any point of the biliary tree. Hilar and node metastasis is a particularly important poor prognostic factor. The incidence of cholangiocarcinoma is increasing globally, currently accounting for ~15% of all primary liver cancers and ~3% of gastrointestinal malignancies. Most patients are diagnosed at an advanced disease stage, which contributes to a 5-year survival of less than 10%. The silent presentation of these tumors combined with their highly aggressive nature and refractoriness to chemotherapy contribute to their alarming mortality, representing ~2% of all cancer-related deaths worldwide yearly [4]. Hilar cholangiocarcinoma (HCCA) is a type of bile duct cancer that occurs in the extrahepatic biliary tree proximal to the origin of the cystic duct. It is the most common malignancy arising from the biliary tract and accounts for two thirds of all CCA diagnoses. The prognosis of CCA is generally poor because early diagnosis is difficult, and most patients present with advanced disease. Surgical resection of initial stage CCA is perhaps the most accepted curative treatment option. We present a case of a patient with intrahepatic/hilar cholangiocarcinoma who has had multiple different interventions, including multiple surgeries, radiofrequency ablation, living donor liver transplantation, recurrence in ribs treated with SBRT. He recurred in the transplanted liver. After many discussions and options, we finally decided to treat him with SBRT in transplanted liver. Due to risk of toxicity, SBRT was delivered on alternate days with five fractions. His follow up imaging revealed a major response in liver lesion. This is the first ever reported case of SBRT in recurrent lesion. In addition, this is the longest survivor of the CCA from India that has ever been reported according to our literary review.
Keywords:Cholangiocarcinoma (CCA); Abdominal Pain
42-year-old Indian male developed symptoms of abdominal pain, belching, nausea, and emesis off and on in 2014. There was no significant past medical history. He had used alcohol off and on and smoked infrequently. He consulted his primary care physician, who ordered an ultrasound of the liver which revealed a mass in the right lobe of the liver that was 61 × 32 mm in size. A PET/CT scan conducted on February 6th, 2015 showed a 46 × 64 mm hypermetabolic lesion in segments IVb and V of the liver with no evidence of metabolically active disease anywhere else in the body. His blood profile was unremarkable, with a normal complete blood count (CBC) and com- prehensive metabolic panel (CMP). His tumor markers were also within normal limits (CA 19-9: 3.96 U/mL; CEA: 2.37 ng/mL). The patient underwent a CT-guided biopsy that reported metastatic adenocarcinoma of the liver. He underwent non-anatomical resection of the liver lesion with gallbladder en bloc, and a removed segment with hepatic artery node and pancreatic node was sent for histopathology. The final pathology report revealed intrahepatic cholangiocarcinoma with elements of hilar involvement too. He was placed on an observation schedule involving scans every 4 months. The patient followed up regularly with his oncologist for almost a year without any evidence of recurrence. He developed asymptomatic radiological recurrence revealing a nodular liver lesion in the segment near the operated bed measuring 14 × 10 mm as well as one lesion which measured 15 × 12 mm in segment II of the left lobe of liver. The PET scan findings were suspicious for recurrent disease, and there was no evidence of metabolically active disease anywhere else in the body. He underwent a bilateral segmental lobectomy in the fall of 2015. Pathology confirmed moderately differentiated cholangiocarcinoma of the liver with lymphocyte infiltrates similar to the original pathology. His subsequent CT scan in February 2016 revealed two small recurrent lesions, one in segment II (9 × 9 mm) and the other in segment IV (10 × 9 mm) of the patient’s liver. He received six cycles of the chemotherapy regimen GEMOX for six months. His PET/CT scan in August of 2016 was normal. He continued with five additional cycles of GEMOX until January 2017, when a repeat PET was normal. He stopped chemo and was placed on an observation schedule. A repeat PET/CT scan on July 5th of 2017 indicated a solitary nodule in the right upper lobe of the lung as well as recurrence of multiple liver lesions–the largest of which was 15 ×15 mm. He resumed chemo with CAPOX in July of 2017. A follow up PET/CT scan in the fall revealed multiple (n = 7) liver lesions in both lobes. There was minimal regression in size and activity compared to the previous scan. He chose to undergo selective internal radiation treatment (SIRT) with yttrium-90 micro- spheres in October of 2017 in Hong Kong. A PET scan performed after this procedure revealed good uptake and no complications. He continued CAPOX for six cycles. A PET/CT scan done in December of 2017 revealed multiple hyper-metabolic lesions in posterior segment I (17 × 13 mm), anterior segment II (11 × 10 mm), and post segment II - IVa (14 × 10mm) indicative of partially treated cholangiocarcinoma. Additionally, a tiny 2 mm non-FDG avid pulmonary nodule- granuloma was present on this scan. In view of multiple recurrences and no evidence of systemic metastatic disease over the course of treatment, the patient transplantation in March of 2018. He had a few minor issues related to infection and thrombosis in the portacaval area that were treated appropriately with antibiotics, stent placement, and anticoagulants. He developed biopsy-proven recurrence in his lungs in July of 2019, for which he started on chemotherapy with nab-paclitaxel, gemcitabine, and cisplatin for six cycles. A PET scan conducted in January of 2020 showed no metabolically active disease in the patient’s body, indicating complete regression. He was on maintenance chemotherapy with nab-paclitaxel and cisplatin for six more cycles. A PET scan conducted in July of 2020 was also negative for metabolically active disease. At this time, he experienced no activity restrictions and remained physically fit. He was then placed on maintenance chemotherapy, with cycles every five weeks in addition to regular follow ups. In January of 2021, a PET scan showed a metastatic lesion in the right 5th rib (5.7 × 3 cm; SUV: 9) and possible metastatic bi- lateral lung nodules with the largest measuring 0.8 × 0.6 cm (SUV: 1.3). He was re- started on chemotherapy and completed five cycles of nabpaclitaxel, gemcitabine, and cisplatin. A PET scan conducted in June of 2021 showed regression in the meta- static right 5th rib lesion (SUV: 4.4) and reduced number as well as size of bilateral lung nodules, the largest of which was 0.6 × 0.3 cm (SUV 1.3). He was treated with single beam radiation treatment (SBRT) over the course of five sessions for the metastatic right rib lesion. He then started on maintenance chemotherapy with nab- paclitaxel, gemcitabine, and cisplatin. His last PET/CT in March of 2022 showed no significant interval changes; the patient is now on increased interval chemo maintenance and is stable without any complaints or limitation of daily activity. He underwent comprehensive genomic profiling (Foundation One) twice and so far we have not discovered any actionable mutations. His subsequent scans revealed recurrence in transplanted liver (see images). By now the patient was getting tired of systemic therapy and was hesitant to consider any more additional systemic chemo. The proximity of his lesion to intestine and also small segment of transplanted liver caused a problem with possibility of irreversible toxicity. Finally, we decided to treat him with SBRT fragmented in five sessions on alternate day bases. He received his treatment between June 2023 and Mid July 2023. His follow up scans revealed near CR in recurrent liver lesion both with reduction in the SUV and size (SBRT treatment planning).
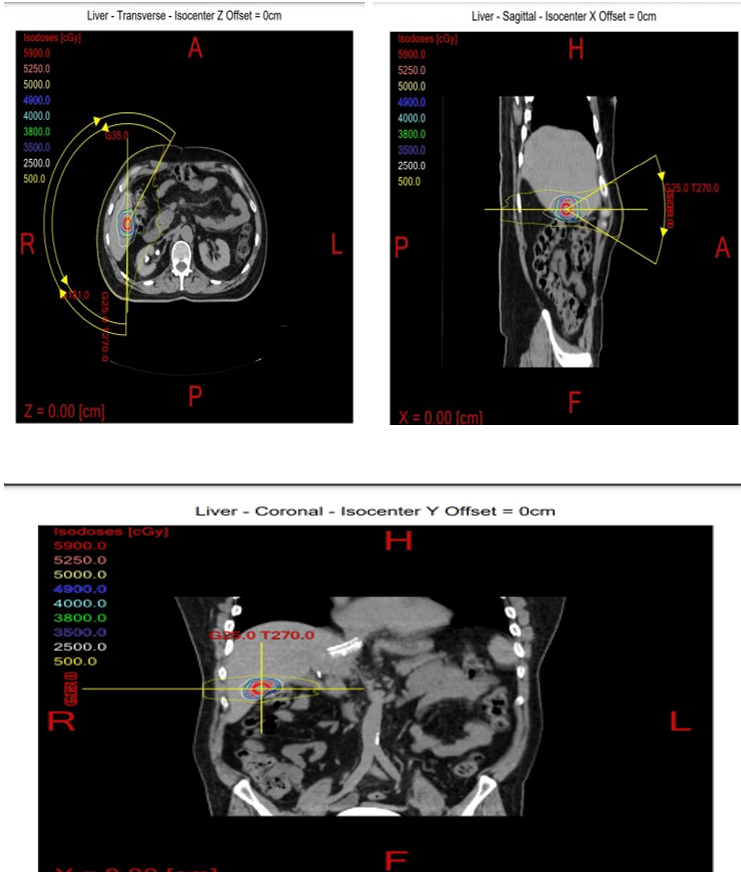
Figure 1
Cholangiocarcinoma is a malignant tumor of the biliary system that can be classified into intrahepatic (iCCA), perihilar (phCCA), and distal cholangiocarcinoma. Treatment options for CCA include surgery [4-6], chemotherapy (either preoperative neoadjuvant or post-operative adjuvant), radiotherapy (SIRT) [7], immunotherapy [8,9], targeted therapy, and liver transplantation [10]. Due to a paucity of cases and the difficulty associated with carrying out large-scale randomized prospective clinical trials, some of the recommended options may have to be individualized, weighing risk and benefit of each approach. Most newer options have been developed only recently, including the role of immunotherapy and targeted therapy that evolved with the advent of precision medicine and comprehensive genomic profiling. Initial studies and research of orthotopic liver transplantation (OLT) for patients with iCCA and phCCA resulted in extremely poor outcomes, and this strategy was abandoned rapidly. However, in the last decade, due to a strict selection process and a neo- adjuvant chemoradiation protocol, OLT has shown promising results in patients with nonresectable phCCA. Intrahepatic cholangiocarcinoma is a growing disease in most countries and can be diagnosed both in cirrhotic and in non-cirrhotic livers. Even though OLT is not performed and rather discouraged in most liver transplant centers, encouraging results have been found in recent investigations analyzing iCCA patients who underwent liver transplantation for a misdiagnosis of hepatocellular carcinoma. There is limited evidence suggesting that patients with early stages of this disease could benefit from OLT. In this review, we analyze the current state-of-the-art treatment of OLT for cholangiocarcinoma as well as new insights and future perspectives. In addition to liver transplantation, within the last four years, research in the disease has been quite promising and a breakthrough came a year ago when the FDA granted accelerated approval to the first targeted therapy for patients with FGFR2 fusion, pemigatinib. In addition, novel drugs against IDH1/IDH2 as well as BAP1, CDK, and ARID1A are rapidly increasing the probability of achieving better outcomes in CCA patients with the appropriate mutation.
CCA is a very difficult cancer to treat and carries a very poor prognosis with median overall survival of 18 months and 5-year overall survival is 11%. Due to paucity of cases and limited options, outside of cases exhibiting actionable mutations, most patients die within 5 years. Our case demonstrates that individualizing treatment options may result in improved survival. He has been treated with Surgery, Adjuvant and Palliative Chemotherapy, Intrahepatic radiofrequency ablation, Orthotopic Liver Transplantation, Radiotherapy and then finally SBRT in the transplanted liver making him the first ever patient treated with multiple interventions that are not deemed applicable to all patients. However, in the era of patient centered cancer care each patient should be assessed for individualized approaches. The current case also demonstrated that SBRT for post-transplant intrahepatic CCA recurrence conferred effective local control without adversely affecting graft function or gut toxicities. A near complete response was achieved in this case.
We report the first ever reported case (to the best of our knowledge) of recurrent cholangiocarcinoma treated with SBRT a rare case of a patient with cholangiocarcinoma who has undergone multiple different interventions that were out of the normal guidelines, ultimately resorting to liver transplantation. He underwent every possible intervention, from multiple surgeries, adjuvant chemotherapy, palliative chemotherapy, selective in- ternal radiation therapy (SIRT), and orthotopic liver transplantation so far with the exception of targeted and immunotherapy. In our literature search, this is one of the few cases of a patient with cholangiocarcinoma who is living beyond eight years with normal performance statu
Copyright: © 2024 Kashyap Patel., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.