Sofia Anais Montilla Soto1*, Ramon Alirio Vergara1, Zener Jose Paez Milano1 and Alfredo Jose Ramirez2
1Coloproctologist Unit, Laparoscopic and General Surgery Department, Hospital Universitario de los Andes, Me rida, Venezuela
2Hepatobiliary and Pancreatic Unit, Laparoscopic and General Surgery Department, Hospital Universitario de los Andes, Me rida, Venezuela
*Corresponding Author: Sofia Anais Montilla Soto, Coloproctologist Unit, Laparoscopic and General Surgery Department, Hospital Universitario de los Andes, Me rida, Venezuela.
Received: September 11, 2024; Published: September 24, 2024
Citation: Sofia Anais Montilla Soto., et al. “Extramammary Paget's Disease. Perianal Paget's Disease Clinical Case” Acta Scientific Cancer Biology 8.10 (2024): 07-09.
Perianal Paget's disease is a rare pathology. It is defined as an intraepithelial adenocarcinoma that affects the perianal apocrine glands, manifests itself with skin lesions with a great morphological variety that can simulate inflammatory conditions, infections or tumors, is diagnosed by taking a biopsy, and surgical treatment and follow-up is the standard procedure, more accepted in these cases. We present the case of a male patient who had a current disease of 1 year of evolution, characterized by color changes and pruritus in the perianal region, who was diagnosed and treated with perianal Paget's disease, presenting an adequate evolution.
Keywords:Extramammary Paget's Disease; Perianal Paget's Disease; Adenocarcinoma
Perianal Paget's disease (PAD) is a low frequency intraepithelial adenocarcinoma of the anal margin, classified as a premalignant lesion being a high grade intraepithelial dysplasia that can degenerate to adenocarcinoma, with capacity for dissemination and high recurrence rate [1], it is part of a subgroup of extramammary Paget's disease (EPEM), it represents 6.5% of extramamammary cases and 1% of perianal neoplasms [2], it can be present under the form; primary which represents a neoplasm of apocrine origin, or secondary a pagetoid dissemination underlying a malignant neoplasm generally of anorectal origin [6]. Clinically there is evidence of erythematous or brownish infiltrated plaque lesions usually with well defined single borders, sometimes edematous with exudates, itching, pain or even asymptomatic, the surface may be rough with lichenification, erosions or crusts that can simulate infectious, tumor or inflammatory lesions [6]. The treatment of choice is surgical resection with lesion free margins, Mohs micrographic surgery can also be used which decreases the recurrence rate [4].
Other alternatives include CO2 laser, topical imiquimod, radiotherapy, cryotherapy and photodynamic therapy but the risk of recurrence is very high reaching 50 to 60% [5]. Its definitive diagnosis is made by anatomopathological studies and immunohistochemistry, by the presence of Paget cells, with ample cytoplasm and clear, arranged in isolation or in groups in all layers of the epidermis and in the cutaneous appendages [6].
We present a clinical case recently attended in our center. It is a 73-year-old male patient, from a rural area, farmer, with no positive pathological history, who presented with a current disease of 1 year of evolution, characterized by color changes and pruritus in the perianal region. On anal inspection (touch and anoscopy), a bilateral exophytic lesion was evidenced, predominantly in the right quadrants, raised, with a warty surface, ulcerated in the central region, not extending into the anal canal, with whitish pseudoliquenoid areas with indurated edges (Figure 1). Initially he was treated with the diagnosis of lichen, received steroids without improvement, therefore an incisional biopsy was performed, with report N.2023-1181 of adenosquamous carcinoma in situ.

Figure 1: Perianal lesion, exophytic, raised, predominantly in the right quadrants.
Rectosigmoidoscopy was performed, ruling out synchronous lesions of the rectum. In the extension studies, abdomino-pelvic tomography did not show positive pathological findings.
He underwent surgery with wide local resection with oncologic margins (Figure 2A) and immediate reconstruction with bilateral V/Y advancement flap (Figure 2B). Currently asymptomatic, after 2 months of follow-up with absence of local recurrence, and adequate healing (Figure 3). The definitive histopathological study reported; adenosquamous carcinoma - Paget's disease, complete resection with tumor free resection margins (Figure 4B).

Figure 2: A) Wide local resection with oncologic margins. B) Bilateral V/Y flap reconstruction with 90% coverage of the defect.

Figure 3: V/Y flap, with adequate healing, without evident lesions. After 2 months of follow-up.
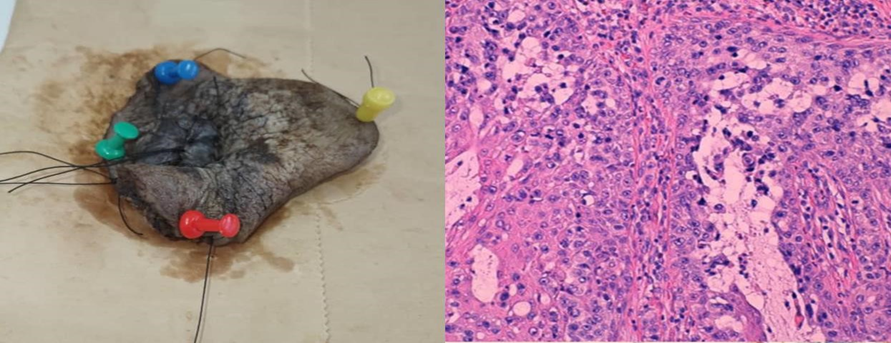
Figure 4: A) Biopsy specimen, disease free margins. B) Pategoid cells, ample cytoplasm, atypical nuclei with small nucleoli.
EPP is a rare pathology, whose incidence is difficult to establish due to the small number of published cases, and there are few cases described in the literature. A multicenter study of EPEM in Korea describes a total of 7 cases of EPP during 5 years, and another study from New York reports 65 patients with EPP in 60 years [3].
PLE should be suspected in any erythematous, scaly and pruritic lesion that does not show response after 6 weeks of topical steroid treatment, and biopsies should be taken for diagnosis.
Due to its low incidence, there is currently no unified treatment protocol, so the choice of management will depend on the type of lesion (primary vs. secondary), the extent and clinical experience. However, wide surgical resection or Mohs micrographic surgery is commonly considered the mainstay of treatment4, being able to reduce recurrence by 25 to 10% [6], because in this type of surgery the operative margins are carefully evaluated by histological studies.
In conclusion, PLE is a rare pathology, in our environment there are few published cases, for its diagnosis should have a high clinical suspicion, due to the wide variety of skin conditions that can originate in the perianal region with greater prevalence, should be confirmed by performing pathological studies, followed by extension studies, to rule out local and visceral dissemination and identify synchronous neoplasms and to establish the best therapeutic option for the patient. Due to their high recurrence rates, despite adequate treatment, follow-up is indispensable in these cases.
Copyright: © 2024 Sofia Anais Montilla Soto.,et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.