Eslam Jalal1, Abubaker Elayis2, Elniema Mustafa1, and Adil Salman3*
1Department of Food Safety and Veterinary Public Health, College of Veterinary Medicine,
University of Bahri
2Department of Medicine, College of Veterinary Medicine, University of Bahri
3One Health Centre, University of Bahri
*Corresponding Author: Adil Salman, One Health Centre, University of Bahri.
Received: August 14, 2024; Published: September 19, 2024
Citation: Adil Salman., et al. “Burden of Food-Borne Bacterial Illness Reported in Emergency Health Centers, Khartoum State, Sudan". Acta Scientific Agriculture 8.10 (2024): 26-31.
This is a retrospective study conducted in Khartoum state during the year 2021 with the aim to identify food poisoning diseases namely: dysentery, typhoid and acute watery diarrhea. The study was designed to cover the years 2016-2020 in government hospitals and health centers in Khartoum State, Sudan. Data was collected from the Department of Emergency Management and Epidemiology of the Federal Ministry of Health in Khartoum State. The study revealed that the mean of food born disease cases visiting the Emergency Department were 29847 compared to 312814 suffering from other diseases during the six years (2016-2021). The highest annual incidence of food-borne diseases per 1,000 inhabitants was 1.1 in 2016, and the lowest was 0.7 in both 2018 and 2019. In 2021, the annual incidence per 1,000 inhabitants dropped to 0.9, and the proportional morbidity rate of food poisoning was 6.5%. The highest annual incidence per 1,000 inhabitants was 1.1 in 2016, and the lowest was 0.7 in both 2018 and 2019. The annual incidence of typhoid in Khartoum State from 2016 to 2021 ranged between 2 and 7 cases per 1,000 inhabitants, with the highest incidence recorded in 2021. The proportional morbidity rate, which represents the percentage of typhoid fever among all foodborne diseases, ranged from 2.7% to 5.3%, with the highest rate also observed in 2021. The morbidity and proportional morbidity rates of watery diarrhea in Khartoum State recorded 0.0% in the years 2016, 2018, 2020, and 2021, while they were 0.01% and 1.17%, respectively, in 2017, and 8.6% and 0.008%, respectively, in 2019. It could be concluded that there were disparities in the studied disease incidences that may warrant further investigation.
Keywords: FBDs; Dysentery; Watery Diarrhea; Typhoid
Food safety refers to the practices and conditions necessary to ensure that food is safe to consume. This encompasses all stages of food production, processing, distribution, storage, and preparation. The primary goal is to prevent food contamination and food-borne illnesses, which can arise from biological, chemical, or physical hazards in food [1]. Food-borne illnesses are a significant public health issue worldwide. The World Health Organization (WHO) estimates that each year, around 600 million people-almost 1 in 10 globally-fall ill after eating contaminated food, resulting in 420,000 deaths [2].
Food safety is a concern worldwide and according to the World Health Organization, developing countries are probably more at risk of foodborne illness because many of these, including those in the Middle East, have limited disease surveillance and prevention and control strategies. Specifically, the Middle East and North Africa [3], more than 100 million people living in this region are estimated to become ill with a foodborne disease every year and 32 million of those affected are children under 5 years. Diarrheal diseases caused by E. coli, norovirus, Campylobacter and nontyphoidal Salmonella account for 70% of the burden of foodborne disease [4]. An estimated 3000 people die each year from unsafe food, caused primarily by diarrheal diseases, typhoid fever, hepatitis A, and brucellosis in the region. Half of the global cases of brucellosis are in people living in this region, with more than 195,000 people infected every year, causing fever, muscle pain or more severe arthritis, chronic fatigue, neurologic symptoms and depression. Cholera, characterized by a short incubation period of 2-5 days and resulting in severe diarrhea and dehydration, is being observed again in countries where public health infrastructure is weakened by conflict, such as Iraq [5]. Many individuals are becoming ill, and some are dying from foodborne diseases.
Many different pathogens and toxins have been identified as causes of food borne diseases and new ones continue to emerge. Prevention may include pasteurization of raw milk, appropriate management of food and proper food canning to reduce food borne diseases [6].
The increasing food safety problems witnessed by Sudan, requires rapid and effective responses. In order to meet this complex public health responsibility, the national capacity to predict and prevent food-borne hazards must be strengthened through public awareness, monitoring and rapidly reacting against outbreaks of food-borne diseases and the occurrence of newly emerging food-borne agents [4].
In developing regions, including parts of Africa such as Sudan, the burden of food-borne illnesses is particularly high due to challenges in food safety management, inadequate infrastructure, and limited access to clean water and sanitation. In Khartoum State, Sudan, these issues are compounded by a lack of awareness and education on safe food handling practices [7].
Cases of food-borne illnesses are rarely investigated in detail and are often underreported. Little is published in peer-reviewed journals or government reports in Sudan, making it difficult to determine the true burden of these illnesses. Available statistics on food-borne diseases in Sudan are not well-analyzed or documented. To improve the situation, national capacity to predict and prevent food-borne hazards must be strengthened through better determination and analysis of the burden of such diseases. The aim of this study was to review food-borne bacterial illnesses and their impact on vulnerable groups reported in emergency medical facilities in Khartoum State covering the years 2016-2020.
The study was conducted in Khartoum state emergency clinics during the year 2021.
This is a retrospective study designed to cover the years 2016-2020 in government hospitals, private hospitals, and health centers in Khartoum State, Sudan.
The specific objective of the study was to identify food poisoning diseases namely: dysentery, typhoid, and acute watery diarrhea.
The process of data collection from the Statistics Department in the Federal Ministry of Health was carried out in an official procedure through a letter from the department of Food Safety and veterinary Public Health, College of Veterinary Medicine, University of Bahri. The targeted departments of the Federal Ministry of Health from which data were collected were Department of Hospital and Specialized Centers (HSC) and Department of Primary Health Care (PHC), Department of Private Treatment Institutions (PTI) and the Department of Emergency Management and Epidemiology (EME). The study focused on identifying cases of food poisoning, dysentery, typhoid, and acute watery diarrhea. Data were sourced from the records of the Statistics and Information Department at the Federal Ministry of Health, obtained through an official request from the Department of Food Safety and Veterinary Public Health at the College of Veterinary Medicine, University of Bahri. Data collection tools included preserved electronic records documenting diseases, the number of affected individuals, the number of deaths, and the dates of reporting. The recorded cases of infection were systematically documented. All records in the EME department were reviewed from files in the archives department for the years 2016-2020.
The process of collecting data took place over three consecutive months, with some difficulties in collecting data such as difficulty accessing sufficient information, the absence of some reports and the missing of parts of the data. With the above-mentioned difficulties in collecting data, additional difficulties were also experienced from the administration of private hospitals such as complicated administrative system, imposing fees for taking data, and lack of complete reports.
Based on the above-mentioned difficulties, the research plan was modified and data were only collected from the EME Department of the Ministry of Health, Khartoum State as EME Department is responsible for counting the number of reported cases of emergency diseases, whether group or individual cases, and counts the number of deaths, if any.
Firstly: a preliminary questionnaire was prepared to obtain information about foodborne diseases, the type of infected person, gender, and the age group (newborn, young child, young person, an adult, or an elderly person). The questionnaire also included the area of infection in which the person was exposed to the disease, the season of infection during the various seasons of the year, and the type of treatment or initial medical treatment steps. When entering the ministry’s system for writing medical reports, we found a model for the report and the data shown in it include the disease, age group, number of infection cases, while the rest of the information must be collected from patient’s file individually.
Secondly: with regards to data collection for food poisoning, dysentery, typhoid, and acute watery diarrhea, the number of infections with these four diseases, the number of deaths, and the total number of infections with other diseases were counted and analyzed using statistical analysis.
A written consent was obtained from the Ethical Research Committee at the Federal Ministry of Health after reviewing the directions set by the committee prior to study conduction.
The collected was data analyzed using statistical packaging for the social sciences (SPSS) Version 23.0 for windows. One sample t. Test, ANOVA test and chi _square test.
As shown in table (1), the annual incidence of food-borne diseases per 1,000 inhabitants in 2016 was 1.1, and the proportional morbidity rate of food poisoning in relation to all cases was 16.5%, which was the highest during the 6 years period. In 2021, the annual incidence per 1,000 inhabitants dropped to 0.9, and the proportional morbidity rate of food poisoning was 6.5%. The highest annual incidence per 1,000 inhabitants was 1.1 in 2016, and the lowest was 0.7 in both 2018 and 2019. This rate is comparable to the 1.22 reported in Ethiopia [3]. In Zimbabwe, the [3] reported an annual incidence of 26.83, which was significantly higher than the incidence reported in this study. This discrepancy may be due to the fact that the data in this study depended solely on cases reported at emergency clinics. A comparable number of an annual incidence per 1,000 inhabitants was 2.2 In Southeast Asia mentioned by [8].
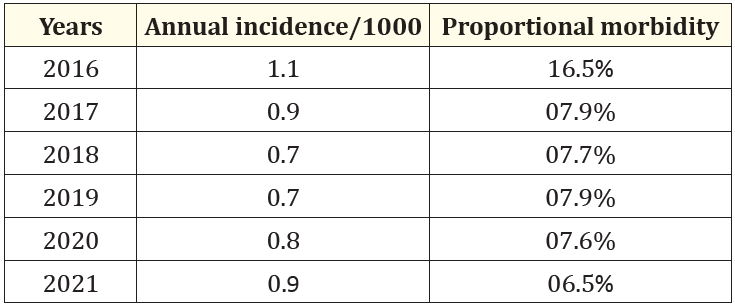
Table 1: Annual incidence per 1,000 inhabitants for food poisoning.
As shown in table (2), the annual incidence of typhoid in Khartoum State from 2016 to 2021 ranged between 2 and 7 cases per 1,000 inhabitants, with the highest incidence recorded in 2021. The proportional morbidity rate, which represents the percentage of typhoid fever among all foodborne diseases, ranged from 2.7% to 5.3%, with the highest rate also observed in 2021 [9]. reported that the annual incidence of typhoid in Sub-Saharan Africa was 1.1 cases per 1,000 inhabitants. The findings in this study are higher, which may be attributed to the high rate of people purchasing ready-to-eat food and the poor quality of water in Khartoum State [10]. Similarly, Mohammed Ahmed., et al. [10] reported a morbidity rate of 5.8 per 1,000 inhabitants in Sudan, which was comparable to the findings of this research. The proportional morbidity of typhoid among all foodborne diseases ranged from 2.4% in 2018 to 5.3% in 2021. The comparison between the mean number of typhoid patients and patients suffering from other foodborne illnesses (FB) visiting the emergency department over the six-year period (2016-2021) shows a notable disparity. Specifically, the average number of typhoid patients was 9761, whereas the average number of FB patients was 2797. This substantial difference was statistically significant, with a p-value of 0.05 obtained using an Independent Samples Test. (table 4). Such a result could point to various factors, including differences in disease transmission, public health measures, or reporting accuracy, among the affected populations.
Further investigation might be warranted to understand the underlying causes of this disparity and to develop targeted interventions to address the higher incidence of typhoid. In Sudan, an unpublished data of Ministry of Health revealed that the incidence of salmonellosis has significantly increased by reporting 43,144 cases and 68 deaths in different hospitals. However, a more accurate figure of salmonellosis is difficult to determine because sporadic cases are under-reported [11].
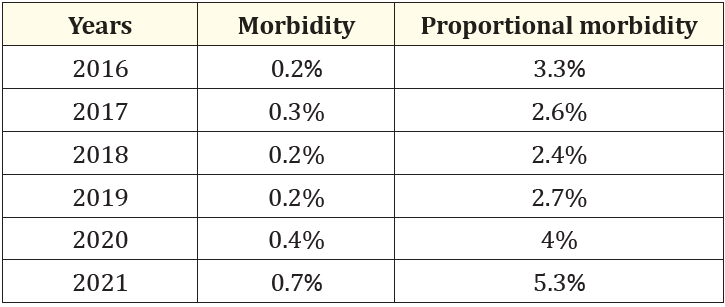
Table 2: Morbidity and proportional morbidity rate of typhoid.
As for watery diarrhea, sometimes referred to as cholera, there were no available data except for the years 2017 and 2019. The morbidity and proportional morbidity rates of watery diarrhea in Khartoum State recorded 0.0% in the years 2016, 2018, 2020, and 2021, while they were 0.01% and 1.17%, respectively, in 2017, and 8.6% and 0.008%, respectively, in 2019, as shown in table 3.
The number of cholera cases was possibly much higher than what is reported in this article due to several amplifying factors, including contamination of water or food sources, climate and extreme weather events, and political and economic crises, which are very evident in the country. Mengel., et al. [12] reported an incidence rate of 0.07% (82,215 cases in 2014 in Africa), which is lower than what was documented in 2017 but higher than that in 2019.
The analysis comparing the mean number of foodborne disease cases to other disease cases visiting the Emergency Department over a six-year period (2016-2021) revealed a significant difference. Specifically, the mean number of foodborne disease cases was 29,847, whereas the mean number of cases for other diseases was substantially higher at 312,814. This difference is statistically significant, with a p-value of 0.05 obtained using an Independent Samples T test. The large difference in the mean number of cases suggests that foodborne diseases constitute a much smaller proportion of the overall emergency department visits compared to other diseases (Table 5).
While foodborne illnesses are a concern, they are vastly outnumbered by other health conditions. Although foodborne diseases are significant, they represent a smaller fraction of total emergency department visits. This indicates that public health resources and interventions might need to prioritize the broader spectrum of diseases causing higher emergency department visits. Nevertheless, food safety remains a critical area to ensure the prevention and control of these illnesses.
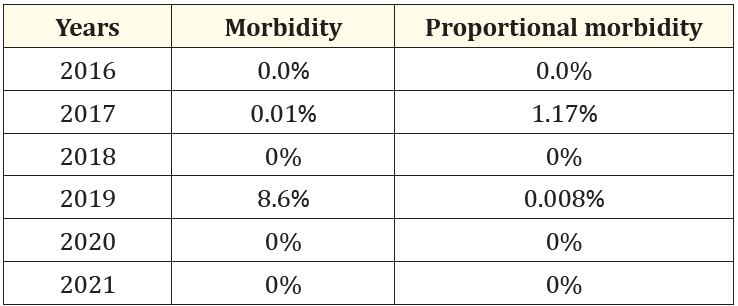
Table 3: Morbidity and proportional morbidity rates for watery diarrhea.
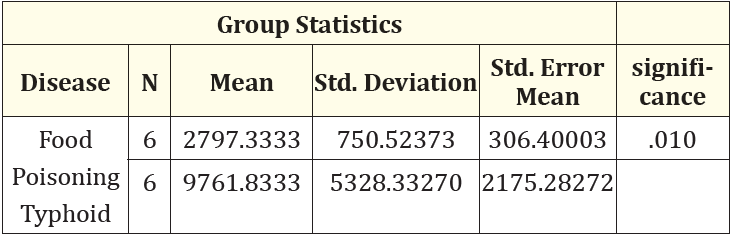
Table 4: The relation between food poisoning cases in general and typhoid in the six years (2016-2021).
The mean of food born disease cases visiting the Emergency Department were 29847 compared to 312814 suffering from other diseases during the six years (2016-2021). The difference between the two other diseases is statistically significant with p=0.05 using Independent Samples Test (Table 5).
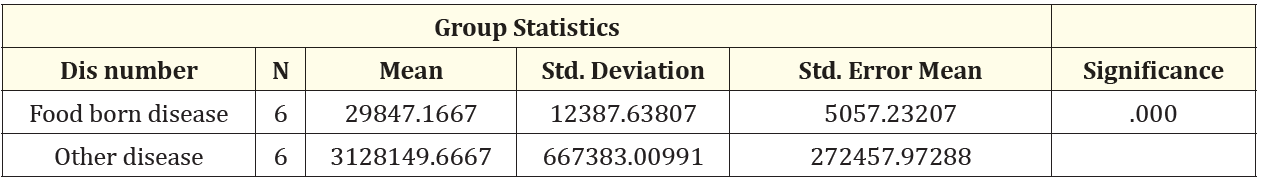
Table 5: The relation between food poisoning cases in relation to other diseases in the six years (2016-2021).
The analysis reveals statistically significant differences in the number of people affected by food poisoning, typhoid, and dysentery over the six-year period (2016-2021), with a p-value of 0.005. (Table 6).
This significant difference highlights the varying impact and prevalence of each disease within the studied timeframe. Understanding these differences can inform public health strategies and resource allocation, and may suggests a tailored interventions to address each disease effectively, considering their unique transmission dynamics, risk factors, and public health implications.
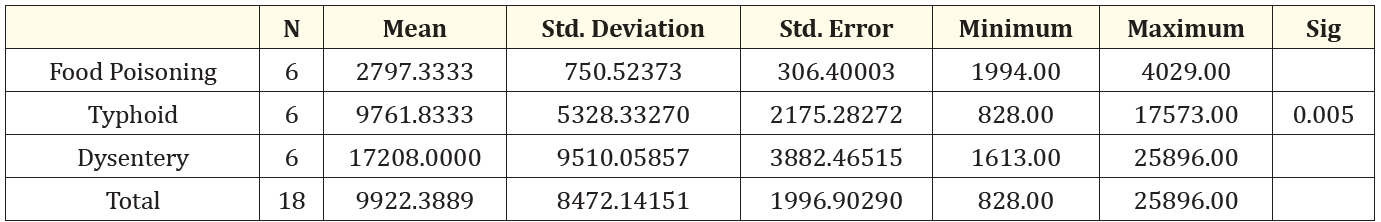
Table 6: The relation between number of food poisoning, typhoid, and dysentery cases during the six years (2016-2021).
The data collected in this study depended solely on cases reported at emergency clinics. This study revealed high incidences of the studied diseases with high disparities which may warrant further investigation. Ministry of Health needs to develop targeted interventions to address the higher incidence of food borne diseases considering their unique transmission dynamics, risk factors, and public health implications.
Copyright: © 2024 Adil Salman., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.