Abtisam Alharam* and Tawfik Abuzalout
Department of General Surgery, Benghazi Medical Center, Benghazi, Libya
*Corresponding Author: Abtisam Alharam, Department of General Surgery, Benghazi Medical Center, Benghazi, Libya.
Received: August 02, 2024; Published: October 21, 2024
Citation: Abtisam Alharam and Tawfik Abuzalout. “Thyroid Abscess: As a Rare Presentation of Follicular Carcinoma Thyroid". Acta Scientific Clinical Case Reports 5.11 (2024):28-31.
Thyroid abscess is an uncommon infection in the neck that affects the thyroid gland and can result in various complications if not managed appropriately. Conversely, it may mask a severe underlying malignancy in conjunction with parathyroid issues.
In our case study, we describe the situation of a 72-year-old woman who was recently diagnosed with primary hyperparathyroidism and was transferred to our surgical department due to acute thyroiditis complicated by an abscess within 4 days, along with a coexisting parathyroid adenoma. The final diagnosis was Follicular carcinoma of the thyroid.
The aim of this case report is to highlight the potentially grave nature of this condition if not promptly identified and treated. Therefore, it is crucial to consider this possibility in the differential diagnosis of acute neck swelling with a high level of clinical suspicion.
Keywords: Acute Thyroiditis; Thyroid Abscess; Follicular Carcinoma
Thyroid abscess in adults is a rare occurrence, particularly in developed countries. When managed with appropriate antibiotic treatment and surgical drainage, it typically has a favorable prognosis [1]. The incidence rate of thyroid abscess is less than 1%, with the left lobe being the primary site of involvement and carrying a high mortality risk if not promptly addressed [2,3]. Staphylococcus aureus is the most commonly identified causative organism [4]. This case report focuses on a unique case of follicular thyroid carcinoma, highlighting the diagnostic challenges and the importance of maintaining a high index of clinical suspicion for effective management.
The patient, a 72-year-old woman with a history of recurrent renal stones and newly diagnosed primary hyperparathyroidism, was transferred to our surgical department under the initial suspicion of a thyroid abscess. She presented with a four-day history of neck pain, sore throat, fever with chills and rigor, and subsequently developed symptoms of neck cellulitis, including a rapid increase in swelling size, along with difficulty breathing and swallowing. The patient had a previous history of a thyroid cyst two years prior. Upon examination, a right-sided neck swelling measuring 7*7*5cm was noted, accompanied by inflammatory skin changes of redness and warmth. Laboratory investigations revealed a leukocyte count of approximately 17 *10^9/L with 79% neutrophils, a CRP level of 790, and normal thyroid function test results (T3: 1.62nmol/L, T4: 82.2 nmol/L, TSH: 3.42 u IU/ml). Kidney function tests showed normal levels, while serum calcium was elevated at 13.3mg/dl, parathyroid hormone was 155 pg/mL, serum phosphate was 2.38 mg/dl, and vitamin D levels were within normal range. A diagnosis of primary hyperparathyroidism was confirmed. A neck ultrasound revealed a large right lobe nodule with cystic degeneration and turbid fluid measuring 7*7*5cm, causing deviation of the trachea to the left, along with skin and subcutaneous tissue inflammation. Further evaluation with contrasted computerized tomography of the neck showed a well-defined cystic lesion measuring 6.6*5.9*5 cm in the right lobe of the thyroid, surrounded by inflamed fat and multiple enlarged lymph nodes bilaterally (Figure 1). A total of 90 cc of pus with blood was aspirated under ultrasound guidance, revealing benign inflammatory cells, predominantly neutrophils, along with a few lymphocytes and red blood cells, indicative of abscess formation. Bacterial culture identified Staphylococcus aureus and Escherichia coli infections. The patient was treated with IV Augmentin 1g for 4 days, followed by IV Meropenem 1g after culture and sensitivity test results.
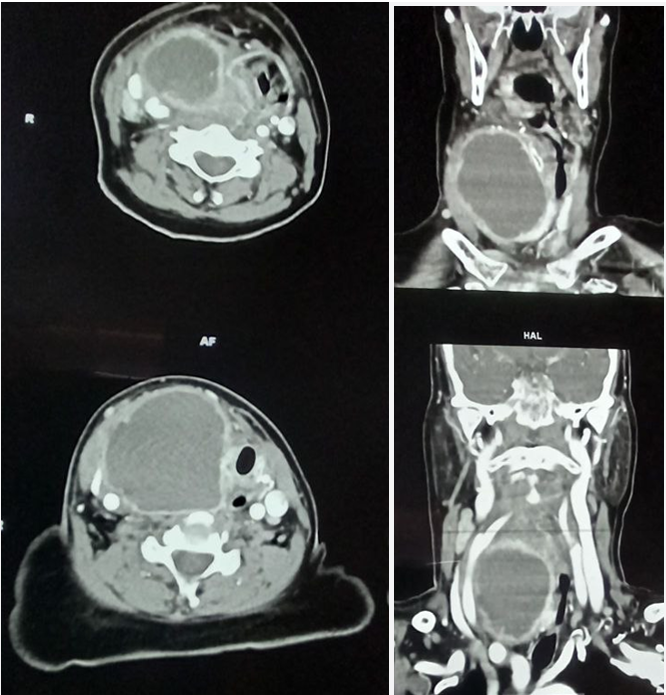
Figure 1: CT Neck with contrast showing well defined cystic lesion measured about 6.6* 5.9*5 cm in the right lobe of the thyroid surrounding with inflamed fat and multiple enlarged lymph nodes bilaterally.
The patient demonstrated a positive response to the resuscitation and Calcimimetic treatment for her primary parathyroid condition. Her condition improved significantly, with the fever resolving and the neck swelling decreasing in size. Following a two-week hospital stay, the patient was discharged in good health. Subsequent isotopic neck and mediastinal scintigraphy (SESTAMIBI) identified abnormal accumulation of radioactive tracer in the left lower parathyroid gland, with no other abnormal findings (Figure 2). Two months later, the patient underwent a right hemithyroidectomy and parathyroidectomy to address the coexisting adenoma, confirming a diagnosis of follicular thyroid carcinoma (Figure 3,4).
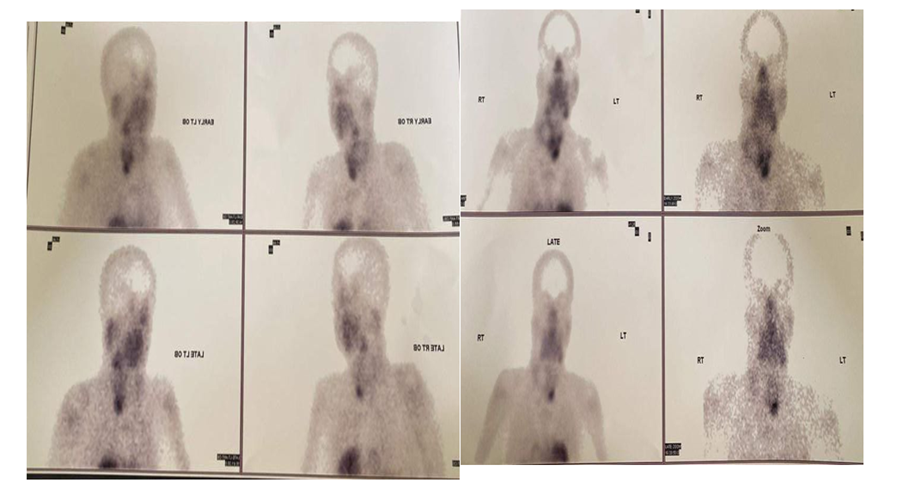
Figure 2: Level of co-localization between mRFP-Vps1 domains and Gga1-GFP. (A) mRFP- Vps1 full length and its truncated species in the first row. Gga1-GFP in the same strain in the second row. The third row shows the merged image. (B) Percentage of cells showing colocalization of mRFP-Vps1 domain to Gga1-GFP carrying endocytic dots.
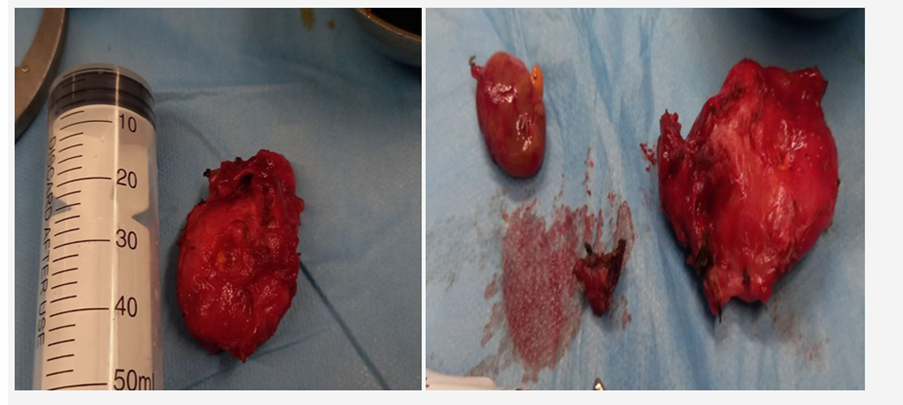
Figure 3: Phytochemical profile of chilli under foliar application of treatments.
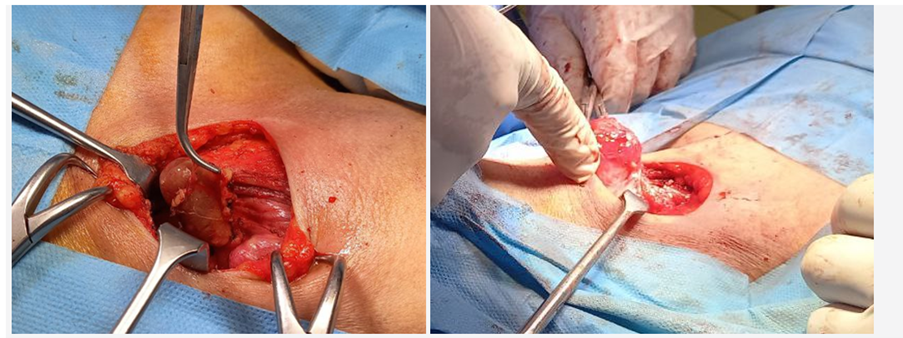
Figure 4: Phytochemical profile of chilli under foliar application of treatments.
The thyroid gland is rarely infected due to various factors, such as its unique histological structure with a high concentration of iodine and a fibrous capsule, as well as its rich venous and lymphatic drainage [5,6]. Infections can be idiopathic or iatrogenic, particularly following fine-needle aspiration cytology. Several risk factors are associated with this condition, including previous thyroid diseases, anatomical anomalies, pyriform sinus, immunocompromised patients, and malignancy [7,8]. Symptoms typically include acute painful neck swelling with elevated inflammatory markers, which can be mistaken for other differential diagnosis [9]. The differential diagnosis of acute bacterial thyroiditis are subacute thyroiditis, thyroid cyst rupture, and infarction of a thyroid nodule [9]. While CT scan and ultrasound of the neck are the preferred diagnostic modalities, they may not always provide conclusive results in the early stages of infection, necessitating a high degree of clinical suspicion [10]. Untreated thyroid infections have a mortality rate of approximately 12%, underscoring the importance of early detection and management [11]. Treatment options range from conservative measures with intravenous antibiotics and aspiration to more aggressive surgical interventions such as multiple incision and drainage or delayed thyroidectomy following resolution of the infection [7,12]. Thyroid abscesses have been reported in numerous cases, some of which have shown concurrent increases in calcium and parathyroid hormones, while others have been the initial presentation of papillary and follicular thyroid carcinoma [8,13-15]. In our case, follicular thyroid carcinoma was presented by thyroid abscess over single thyroid lesion with association of parathyroid adenoma and primary hypercalcemia at the same time of presentation. The Infection was caused by multiple organisms, including Staphylococcus aureus and Escherichia coli, in a patient with a history of previous thyroid pathology. This infection led to an increase in parathyroid and calcium levels, which had not been previously documented as indicative of parathyroid adenoma. Computed tomography and ultrasound proved to be reliable tools for assessing the condition, and conservative management with intravenous antibiotics and ultrasound-guided aspiration effectively alleviated symptoms until surgical intervention could be performed. Ultimately, a definitive diagnosis of follicular thyroid carcinoma was established.
Thyroid abscess represents an uncommon manifestation of neck swelling. Simple cases can be effectively managed through conservative measures. Nevertheless, it is crucial to bear in mind that thyroid abscess could potentially mask a challenging scenario of follicular thyroid carcinoma. Therefore, clinicians should maintain a high index of suspicion for this malignancy in cases of acute neck infection, particularly in elderly individuals with persistent and progressive symptoms.
Written informed consent for the case to be published (including images, case history and data) was obtained from the patient for publication of this case report.
Copyright: © 2024 Abtisam Alharam and Tawfik Abuzalout. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.