Križaj Julija, Frangež Igor and Dajoski Kliment*
Department for Surgical Infections, University Medical Centre Ljubljana, Slovenia
*Corresponding Author: Dajoski Kliment, Department for Surgical Infections, University Medical Centre Ljubljana, Slovenia
Received: October 03, 2024; Published: October 15, 2024
Citation: Dajoski Kliment., et al. “The Use of Curea P1 DUO Active and Curea P2 Active Wound Dressings for the Treatment of Chronic Wounds". Acta Scientific Clinical Case Reports 5.11 (2024):15-21.
Effective wound management is a crucial aspect of healthcare, mainly focusing on restoring skin integrity, minimizing complications and enhancing the patient's quality of life. Treatment of both acute and chronic wounds typically requires timely interventions, followed by the application of an appropriate dressing to protect the wound site and create optimal healing conditions. Chronic wound management often requires the use of advanced care products such as specialized dressings, negative pressure wound therapy and various skin substitutes, accompanied by the treatment of associated morbidities to enable successful long-term treatment outcomes. Curea dressings represent a novel approach to the management of chronic and malignant wounds with significant exudate production. These multipurpose dressings incorporate innovative materials and technologies to optimize the healing process, efficiently transfer and retain exudate and enhance patient comfort during dressing changes. In our case study we present four case reports following patients admitted at the Department for Surgical Infections for treatment of chronic wounds of various etiologies, all exhibiting abundant amount of discharge. Using the curea P1 DUO active and curea P2 active dressing, specifically designed for the multifaceted challenges of wound care, we observed a decrease in wound size, absence of bacterial colonization and a complete elimination of malodour in all four patients. Our findings, supported by the literature, indicate that curea P1 DUO active and curea P2 active dressings provide a clinically efficient, cost-effective and patient-friendly treatment option for heavily colonized or infected chronic ulcers with high exudate secretion.
Keywords: Wound Management; Chronic Wounds; Modern Coating with Activated Charcoal; Curea Dressings; Exudate Management; Bacterial Colonisation
TMT: Transmetatarsal; CRP: C-reactive protein
The management of both acute and chronic wounds presents a critical aspect of healthcare. The main goal of treatment is to restore the integrity of the skin and underlying tissues, minimize complications and improve the patient's overall quality of life [1]. It involves various strategies and techniques aimed at promoting healing, preventing infections as well as minimizing pain and scarring [2]. Acute wounds, such as surgical incisions, lacerations and burns generally follow a predictable healing process and respond well to timely and appropriate interventions. Treatment of these wounds typically involves debridement of necrotic tissue and achieving hemostasis, followed by an application of a dressing that protects the wound site and creates optimal wound healing conditions [3]. In contrast, chronic wounds, such as diabetic, ischemic, pressure and venous leg ulcers, often result from the presence of underlying health conditions and present as persistent challenges due to their prolonged and complicated pathogenesis. Treatment strategies often involve the use of advanced wound care products like specialized dressings, negative pressure wound therapy and various skin substitutes, along with the management of accompanying morbidities to achieve successful long-term outcomes [4].
In polymorbid patients, critical bacterial colonization and infection can significantly impede wound healing, often prolonging the inflammation phase and leading to the development of chronic wounds. These wounds are typically colonized by polymicrobial pathogens that form biofilms, which prevent healing [5]. In such cases, clinical guidelines recommend surgical excision and debridement of necrotic tissue, along with prolonged antibiotic therapy based on microbiological analysis to completely eradicate the infection and enable healing [6]. Additional procedures are available, such as ultrasound debridement or antiseptic irrigation, and the use of modern antimicrobial dressings, which are crucial for promoting effective wound healing [7].
Advances in wound care technologies and a deeper understanding of wound healing physiology continue to enhance treatment effectiveness, offering potential for better recovery and a reduced incidence of chronic wounds. Choosing an effective wound dressing is essential for managing excess exudate and maintaining a moist wound bed along with preventing peri-wound maceration [8].
Curea dressings (curea medical GmbH, Heilbad Heiligenstadt, Germany) are new multipurpose wound dressings designed for the management of chronic and malignant wounds characterized by low to significant exudate production. The dressing incorporates innovative materials and technologies that optimize the wound healing process. The core of the curea dressing is the patented SuperCore® technology, which consists of natural cellulose fibres and sodium polyacrylate. The unique bonding allows the dressings to efficiently transfer and retain exudate through the force of capillary action. Curea dressings are also composed of layers of polypropylene fibres or polyethylene mesh to prevent adherence to wounds and enhance the comfort during dressing changes. They are effective in managing moisture by creating and maintaining a moist wound bed, which is crucial for promoting the formation of granulation tissue and epithelialization. Additionally, curea dressings exhibit high absorbency, efficiently absorbing excess exudate including blood and bacteria, while minimizing the risk of maceration. Another important property of curea dressings is odour control. Some curea dressings incorporate activated charcoal, which helps reduce unpleasant odours often associated with chronic wounds, improving patient comfort and overall quality of life [9]. Furthermore, curea dressings contribute to reducing the bacterial burden in wounds, creating a cleaner wound environment and lowering the risk of infection. Due to their high absorbency and moisture-retentive properties, curea dressings can be worn for extended periods of time, requiring fewer dressing changes. This not only minimizes disruption to the wound bed but also reduces overall treatment costs [10].
There are several varieties of curea dressings, including curea P1, curea P2, curea P1 DUO, curea P1 DUO active, and curea P2 active. Each type of curea dressing is tailored to address specific wound characteristics in various stages of healing. Curea P1 is optimal for soft debridement of wounds in the early inflammatory phase with heavy exudate, providing effective absorption and moisture retention. Curea P2 active incorporates a non-adherent layer to enhance patient comfort during dressing changes and is designed for wounds with low to high amounts of exudate. Additionally, curea P1 DUO and curea P1 DUO active can be applied from either side, making them ideal for wounds with abundant exudate and associated odors [9].
In our case study, we present a series of 4 case reports following patients admitted at the Department for Surgical Infections for the treatment of chronic wounds of various etiologies, all exhibiting an abundant amount of exudate production. They were all treated using curea dressings, specifically designed to address the multifaceted challenges of wound care, providing effective exudate management, infection control and creating ideal wound healing conditions. One patient was treated using curea P1 DUO active, while the other three patients received treatment with curea P2 active.
62-year-old Caucasian male with diabetes mellitus type 2 was admitted to the Department of Surgical Infections for operative management of a gangrene of the left lower limb. After admission, transmetatarsal (TMT) amputation was performed along with radical debridement of the calcaneus region. Prior to the procedure, wound swab samples were obtained for microbiological analysis. The results revealed a soft tissue infection with four different types of bacteria, all sensitive to antibiotic treatment with Imipenem. After consulting the infectologists, the patient received the appropriate antibiotic therapy. Following the procedure, the wound measured 12 cm in height and 8 cm in width (Figure 1). Granulation tissue was visible in the bottom of the wound, with surrounding area of necrosis in the borders. Exudate was present in moderate amounts, exhibiting a foul odour.
Three weeks after performing consecutive dressing changes with curea P1 DUO active dressing the wound measured 10,5 cm in height and 4,8 cm in width.
Four weeks after the procedure the wound continued to successfully heal, measuring 5 cm in height and 4 cm in width (Figure 2). The wound bed was covered with granulation tissue, with epithelisation present on the borders of the wound. Another wound swab sample was obtained and sent to microbiology for analysis. The results revealed a complete absence of pathogens.
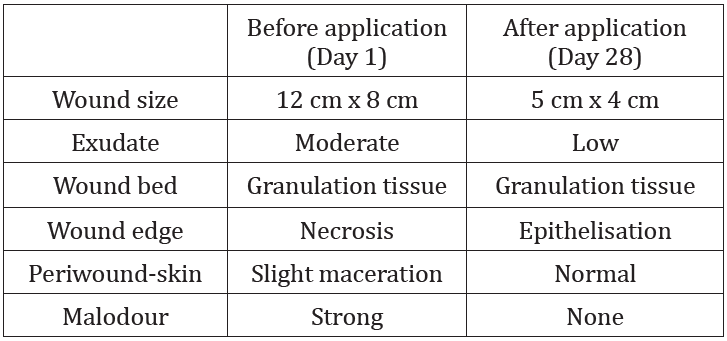
Table 1: Case report 1: Wound status of the patient before and after treatment with curea P1 DUO active.
68-year-old Caucasian male with diabetes mellitus type 2, who previously underwent TMT amputation of the fourth and fifth toe of the left foot, presented in the Emergency room with fever and pain in the operated region (Figure 3). Laboratory findings showed an increased level of C- reactive protein (CRP) of 38 mg/L. Microbiological analysis of the swab sample revealed a soft tissue infection withnterococcus faecalis and Prevotella melaninogenica. After admission, debridement of necrotic tissue and revisional TMT amputation of the fourth and fifth toe was performed. The patient also received antibiotic treatment based on antibiogram results. After the procedure, clinical examination showed a wound bed covered with granulation tissue and a small amount of fibrine. The surrounding skin was erythematous, tender to palpation. The wound measured 4,5 cm in height and 2,8 cm in width.
Four weeks after the initial examination, the wound measured 3,2 cm in height and 1,8 cm in width (Figure 4). Furthermore, repeated microbiological analysis showed that pathogens were no longer present in the wound.
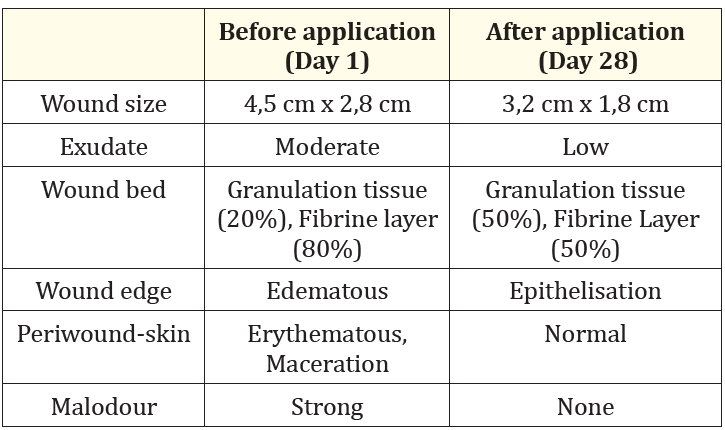
Table 2: Case report 2: Wound status of the patient before and after treatment with curea P2 active.
28-year-old healthy Caucasian male presented in the Emergency room with fever and malaise following a traumatic injury in the right lumbar region. Haemathoma and oedema of the injured area were visible, tender to palpation. Laboratory tests were performed, showing an increase in values of CRP of 271 mg/L and leucocytes of 25,3 × 10-9. Infectologists recommended antibiotic treatment with amoxicillin and clavulanic acid. After the admission, debridement of necrotic tissue was performed and intraoperative swab samples were obtained (Figure 5). Microbiological analysis revealed an infection with Streptococcus pyogenes. Due to a purulent hemorrhagic discharge present a day after the initial procedure, a revision debridement was performed. Repeated laboratory analysis revealed a decrease in inflammation markers with CRP values of 132 mg/L and leucocytes of 11,4 × 10-9. Two days after the revision procedure the wound presented with signs of granulation tissue formation, covered by a layer of fibrine with moderate amount of discharge. The wound measured 2 cm in height and 6 cm in width.
Seven days after the procedure, the wound bed was covered with granulation tissue, the discharge was minimal, and the surrounding skin showed no signs of inflammation. At the examination, the wound measured 1 cm in height and 4,5 cm in width. Only 12 days after being discharged, the wound was completely healed and the patient had no subjective complaints (Figure 6).
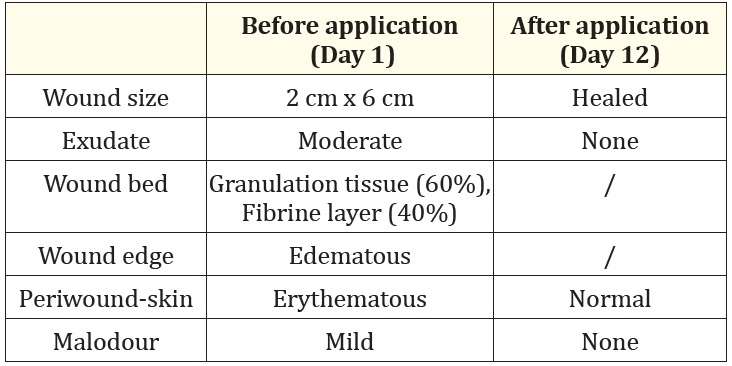
Table 3: Case report 3: Wound status of the patient before and after treatment with curea P2 active.
70-year-old Caucasian male with diabetes mellitus type 2, arterial hypertension and peripheral artery disease was admitted to the Department for Surgical Infections for treatment of a chronic ulcer. The wound was present in the palmar region above the first metatarsophalangeal joint of the left foot (Figure 7). Prior to the admission, the patient underwent TMT amputation of the fourth and fifth toe of the left lower limb. At clinical examination, the wound measured 5 cm in height and 4 cm in width. The wound bed was covered in fibrine with some granulation tissue formations, accompanied by heavy amounts of exudate. Surrounding hyperkeratosis was present. Wound swab sample revealed a tissue infection with an Enterobacter cloacae. After consulting infectologists, the patient received antibiotic treatment with ciprofloxacin and linezolid.
Seven days after the procedure the wound measured 3,5 cm in height and 3 cm in width. After 42 days the wound showed formations of granulation tissue and epithelisation present on the borders. It measured 3 cm in height and 2 cm in width (Figure 8).
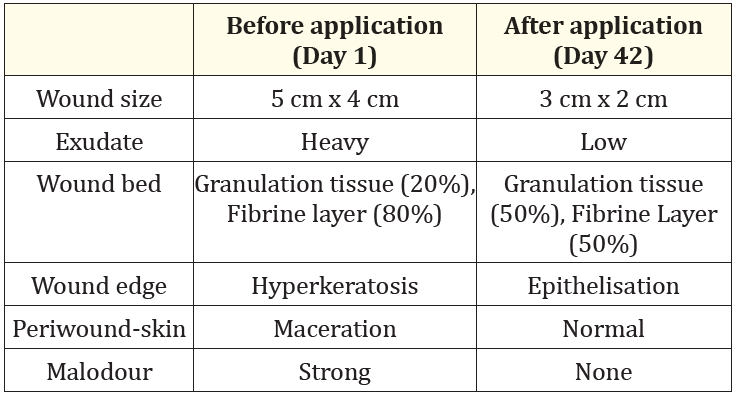
Table 4: Case report 4: Wound status of the patient before and after treatment with curea P2 active
Our case study was designed to investigate the efficiency and determine potential advantages of using curea P1 DUO active and curea P2 active dressing in the treatment of heavily colonized or infected chronic ulcers with high exudate secretion. When designing the case study, we anticipated a reduction in bacterial burden and a decrease in maceration of the surrounding skin. Furthermore, we expected that wound healing would be accelerated as a result of the dressings' ability to absorb and retain exudate. Another anticipated benefit was the elimination of unpleasant odour associated with chronic ulcers. Based on our hypotheses, we also anticipated the use of curea P1 DUO active and curea P2 active dressing to demonstrate cost-effectiveness compared to standard wound care products. By investigating these outcomes, we aimed to provide evidence supporting the clinical benefits and economic advantages of utilizing curea dressings in the management of chronic ulcers with high exudate secretion.
Multiple studies were conducted comparing the efficiency of various dressing types in retaining excess exudate. A study by Orlov., et al. compared the exudate retention properties of foam-based dressing compared to dressings containing superabsorbent polymers on a robotic leg system with two venous leg ulcers. They found that dressings containing superabsorbent polymers were more efficient in retaining excess exudate compared to foam-based dressings. However, notable differences in fluid handling performance were observed between the various superabsorbent polymer dressings [11]. Another study by Orlov., et al. further compared fluid retaining properties between superabsorbent polymer dressings and multipurpose dressings. They found multipurpose dressings, such as curea dressings, were the most efficient in retaining excess exudate [12].
Two case studies performed by curea medical found that the use of multipurpose curea dressings resulted in reduction of bacterial burden by binding and inactivating bacteria present in the wound, without causing the development of antibiotic resistance. They described a significant reduction in wound odour following a single application of the curea dressing and complete absence of unpleasant smell later in the course of treatment. Due to its high absorbance properties and a consequential reduction in dressing change intervals, curea dressings proved to be a cost-effective treatment option [13,14].
A randomized study by Probst., et al. included 77 patients with chronic wounds of various etiologies. They compared the efficiency of treatment with curea P1 DUO active and silver-containing non-adhesive hydrocellular foam dressing Allevyn Ag. The results showed a two times faster reduction in wound size and a significant decrease in maceration following treatment using curea P1 DUO active dressing. Due to the longer application period of curea P1 DUO active desired wound rest is achieved, allowing the improvement of wound healing process [15].
In our case study, by utilizing the curea P1 DUO active and curea P2 active dressing, we confirmed the efficiency of the superabsorbent core to retain excess exudate, with the observed reduction of exudate production as well as the absence of surrounding skin maceration in all four patients. A complete reduction in bacterial burden was also observed, although it is imporant to consider that all of the patients received additional specific antibiotic treatment based on the microbiological analysis results. Due to the expected positive effect of curea dressings on the wound healing process, we reported a significant decrease in wound size, observed in all four patients. Longer application period of the dressing proved to be favourable not only for the promotion of the healing process, but for the patient directly, requiring fewer dressing changes, during which they reported no pain was present. Based on the observed results of our case study supported by the evidence of existing literature, we found that utilizing curea dressings in everyday practice proved to be efficient in accelerating the healing process, patient friendly and a cost-efficient method in the treatment of heavily colonized or infected chronic ulcers with high exudate secretion. However, additional studies involving a control group are necessary to conduct a more precise evaluation of the direct impact curea P1 DUO active and curea P2 active dressings have on treatment outcomes.
Our case study demonstrated that curea P1 DUO active and curea P2 active dressings are highly effective in managing heavily colonized or infected chronic ulcers with significant exudate production. The findings of the study showed that the dressings not only reduced wound size and bacterial colonization but also eliminated malodour and prevented maceration of the surrounding skin. This indicates that both curea P1 DUO active and curea P2 active dressings help create an optimal healing environment as well as improve the patients' comfort. Moreover, the dressings proved not only to be clinically effective but also demonstrated financial efficiency. Their high absorbency and extended wear time reduced the frequency of dressing changes, minimizing material consumption and overall treatment costs without compromising the quality of care. Our case study, supported by the literature, emphasize the clinical effectiveness of curea P1 DUO active and curea P2 active dressings by providing a practical and cost-efficient solution for enhancing wound healing. The evidence provided supports the utilization of the studied dressings in routine clinical practice for effective management of colonized or infected chronic ulcers with significant exudate production.
We have no conflict of interest or financial interest to declare.
Copyright: © 2024 Dajoski Kliment., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.