Aboubekr Fadlallah, Senouci Oum Elkheir Soltana*, Kerras Meriem Elbatoul, Bedjaoui Hind, Tachema Ikram and Messaoud Mimou
Department of Gynecology and Obstetrics, Mother and Child Hospital of Sidi Bel Abbes, Taleb Morad Faculty of Medicine – Djillali Liabes University, Algeria
*Corresponding Author: Senouci Oum Elkheir Soltana, Department of Gynecology and Obstetrics, Mother and Child Hospital of Sidi Bel Abbes, Taleb Morad Faculty of Medicine – Djillali Liabes University, Algeria.
Received: September 20, 2024; Published: October 14, 2024
Citation: Senouci Oum Elkheir Soltana., et al. “Transvaginal Cervico-Isthmic Cerclage Using Polypropylene Tape: Surgical Procedure and Pregnancy Outcome. Fernandez Procedure". Acta Scientific Clinical Case Reports 5.11 (2024):10-14.
Objective: Evaluate the efficacy of cervico-isthmic cerclage with a vaginally placed synthetic tape in women at high risk of preterm delivery.
Patients and Methods: This was a case series evaluation of 07 women who underwent vaginal cervico-isthmic cerclage with placement of a synthetic tape, performed at the Sidi Bel Abbès mother-child specialized hospital between June 2023 and June 2024. These women were all at very high risk of preterm delivery: multiple late spontaneous abortions, history of failure of conventional cerclage (McDonald). Cervico-isthmic cerclage was performed between 12 and 14 weeks of amenorrhea, with vaginal placement of a polypropylene band at the cervico-isthmic junction.
Results: The mean age of these patients was 29.1 years (range 22-39 years). No complications were observed during the operation. The average operating time was 40 minutes (± 5.1) (extremes 35-45 min). For delivery, Caesarean section was systematic in all patients, given that this type of cerclage is intended to be permanent. The average term of delivery was between 36 and 37 weeks of amenorrhea. The newborns had an average birth weight of 2,900 g (± 500). The late abortion rate was 16.66% (1/6). In two cases, the tape had to be removed secondarily when superinfection was discovered. To date, one patient is pregnant at 22 weeks of amenorrhea, with no signs of preterm delivery.
Conclusion: Cervico-isthmic cerclage with vaginal placement of a synthetic tape is a minimally invasive alternative to abdominal cerclage with similar efficacy in women at high risk of preterm delivery.
Keywords: Synthetic Tape; Cervical Incompetence; Cerclage; Cervix; Preterm Delivery; Fernandez Technique
Preterm birth is the main cause of perinatal mortality and morbidity [1]. In France, they account for 7.2% of all deliveries [2]. Several authors have shown that cerclage has a significant role in preventing preterm delivery before 34 weeks of amenorrhea (SA) [3,4].
However, a recent meta-analysis by the Cochrane, based on 7 randomized studies, weighted these conclusions regarding the efficacy of cerclage. In fact, this is only beneficial for women with a very poor obstetrical prognosis, i.e. those with a very high risk of late miscarriage (in the second trimester) due to cervical incompetence [5]. This cervical incompetence affects approximately 0.1 to 1% of all pregnancies [6].
Another recent meta-analysis published by Berghella., et al. concludes that cerclage appears to reduce the rate of prematurity in women with a history of preterm delivery and a shortened cervix [7].
We propose a vaginal cervico-isthmic cerclage technique in which we replace the cerclage thread with a synthetic polypropylene tape. In our view, this technique combines the simplicity of the vaginal route with the efficacy of cervico-isthmic cerclage compared with conventional cervical cerclage. The aim of this study was to study the results of this technique in women at very high risk of preterm birth.
Between June 2023 and June 2024, 07 women underwent cervico-isthmic cerclage because of their very high risk of preterm delivery. The indication for cerclage was the observation of multiple late spontaneous abortions associated with a history of conventional cerclage failure (McDonald).
For the 07 patients, cervico-isthmic cerclage was performed between 12 and 14 weeks of amenorrhea. The mean age of the patients was 29.1 years (ranging 19 to 40 years).
All our patients were nulliparous. all our patients had a history of repeated late spontaneous abortions and a history of failed conventional cerclage (McDonald technique).
Cerclage was performed after the first ultrasound scan, usually prescribed at 12 weeks of amenorrhea.
Ultrasound measurement of cervical canal length for the 07 patients measured by endo-vaginal ultrasound before cerclage was less than 25 mm.
Cervico-isthmic cerclage using the Fernandez technique. The mode of anesthesia was locoregional with spinal anesthesia. The cervix is grasped with 2 Pozzi forceps placed on the anterior and posterior edges. The colpotomy is performed in a semicircular way anteriorly and posteriorly at the cervicovaginal junction. The incisions are 2 to 3 cm long and not confluent. The bladder is dissected, then reclined from the anterior aspect of the cervix using a narrow vaginal valve. This bladder dissection is continued along the midline until the cervico-isthmic junction is exposed. Posteriorly, after a brief dissection, the rectouterine pouch is opened with the scissors, exposing the utero-sacral ligaments and the posterior aspect of the cervico-isthmian junction.
The special feature of this technique is that a non-absorbable thread is replaced by a synthetic tape.
The synthetic tape is then placed on either side of the cervico-isthmic junction, above the insertion of the utero-sacral ligaments and below the level of the uterine artery junction (which can be palpated between two fingers).
The tape is put in place once passed, around the isthmus, the tape is tightened and secured to the isthmus with a non-absorbable polypropylene thread.
The peritoneum of the rectouterine pouch and the vaginal mucosa are sutured with absorbable thread.
After the operation, tocolysis is systematically instituted for a minimum of 48 hours. Women are then monitored clinically, ultrasonographically and biologically.
Vaginal cervico-isthmic cerclage was possible in all 07 women. The average operating time was 40 minutes (±5.1) (extremes 35-45 min) and the average hospital stay 1.4 days (± 0.5).
No intraoperative complications were observed. There were no bladder injuries and none of the 07 women experienced haematuria after the operation.
At the time of this article, 01 patient is pregnant at 22 weeks of amenorrhea. She has not yet been re-hospitalized, nor has she shown any signs of threat of late abortion. For the others, delivery by caesarean section took place between 36 and 37 weeks of amenorrhea. The newborns had a mean birth weight of 2,900 g (± 500). No neonatal deaths were recorded.
Delivery before 32 weeks of amenorrhea occurred only once.
Two patients presented a superinfection and not an abscess of this tape, 03 months for the 1st patient and 6 months after delivery for the second patient. The tape was removed, allowing symptoms to disappear rapidly under antibiotic treatment.
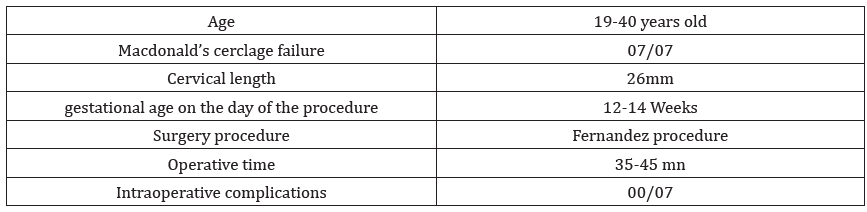
Table 1: Obstetric History and Course of Cervico-isthmic Cerclage with Vaginal Tape.
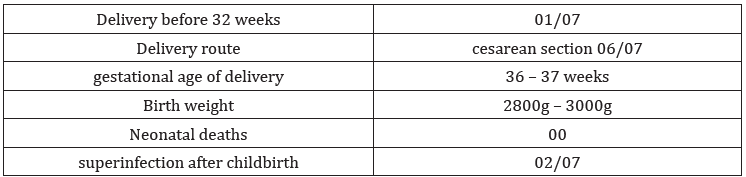
Table 2: Obstetrical outcome before and after cervico-isthmic cerclage with vaginal tape.(history and outcome with 06 women who delivered).
This technique of cervico-isthmic cerclage with vaginal placement of a polypropylene tape is a new method in the prevention of preterm delivery in women at high obstetrical risk. Placement of this non-absorbable tape above the level of insertion of the utero-sacral ligaments at the cervico-isthmic junction perfectly mimics the abdominal cervico-isthmic cerclage described by Benson and Durfee, which has proved effective in women at high risk of preterm birth [11].
Several studies have shown that the technique described by Benson and Durfee is effective in most women with cervical incompetence, for whom conventional cerclage would be ineffective or impractical [13-15].
In a literature review, Zaveri., et al. compared obstetrical outcomes after abdominal cervico-isthmic cerclage versus conventional cerclage techniques, in women who had failed cerclage in a previous pregnancy [19]. They concluded that this abdominal cervico-isthmic cerclage was associated with a lower risk of perinatal death or very preterm delivery before 24 weeks of amenorrhea, but that this type of cerclage could be associated with a high rate of operative complications [19]. Moreover, when removal of this type of cerclage becomes necessary, a new laparotomy (or laparoscopy) must be performed [20,21]. The good obstetrical results (a single delivery before 32 weeks of amenorrhea and 76% of deliveries between 36 and 37 weeks of amenorrhea) and the neonatal survival rate observed in our series are comparable to those reported in studies using abdominal cervico-isthmic cerclage. Delivery rates after abdominal cerclage range from 85% to 90% [12-19].
Katz and Abrahams recently reported a technique for vaginal cervico-isthmic cerclage, but without placement of a prosthetic band [22]. They observed a 100% fetal survival rate in their series of around fifty patients. In this series, the preterm delivery rate before 32 weeks of amenorrhea was 32% and the rate of deliveries before 30 weeks of amenorrhea was 21%. In our population, the preterm birth rates observed were lower, although we cannot directly compare these 2 series.
Katz and Abrahams recently reported a technique for vaginal cervico-isthmic cerclage, but without placement of a prosthetic tape [22]. They observed a 100% fetal survival rate in their series of around fifty patients. In this series, the preterm delivery rate before 32 weeks of amenorrhea was 32%, and the delivery rate before 30 weeks of amenorrhea was 21%. In our population, the preterm birth rates observed were lower, although we cannot directly compare these 2 series.
Other authors such as Golfier., et al. had previously described other cervico-isthmic cerclage techniques without the use of a synthetic band, and reported results comparable to those of Katz and Abrahams [22,23].
These vaginal cervico-isthmic cerclage techniques using simply a non-absorbable thread are no less risky: these authors report significant complications such as a bladder wound, a subvesical hematoma and urinary retention. We chose to use a synthetic band to improve perinatal results after cerclage in women at very high risk of preterm delivery. The sclerosis caused by the presence of prosthetic material is likely to increase cervico-isthmic resistance to uterine contractions. This hypothesis is supported by the low rates of preterm delivery observed in our study compared with those observed in the study by Katz and Abrahams, where only non-absorbable thread was used for cerclage (although only a comparative study could confirm this hypothesis).
The fact that the tape is placed vaginally makes it easier to remove when necessary, for example in the event of erosion or infection. This type of complication is known to occur with vaginally-placed synthetic tape, and its management is generally simple. Among our patients, two cases of superinfection were observed. After removal of the tape, symptoms rapidly disappeared.
We decided to carry out a systematic caesarean section at 37-38 weeks of gestation before the onset of work, as a caesarean section before the onset of work is associated with a low complication rate [26].
This cerclage may be useful for a subsequent pregnancy.
Cervico-isthmic cerclage with vaginal placement of a synthetic band is an effective alternative to abdominal cervico-isthmic cerclage in women at high risk of preterm delivery.
Two main indications can be identified:
on the one side, women with a history of late spontaneous abortion and a history of conventional cerclage failure; and on the other side, women with a highly abnormal cervix preventing conventional cerclage.
Further studies involving a larger number of cases will be needed to determine the benefits of this new type of cerclage for subsequent pregnancies.
Copyright: © 2024 Senouci Oum Elkheir Soltana., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.