Ramazan Uçak*, Omer Faruk Dilbaz, Nedim Polat and Mehmet Resit Asoglu
Department of Pathology, University of Health Sciences, Sisli Hamidiye Etfal Teaching and Research Hospital, Istanbul, Turkey
*Corresponding Author: Ramazan Uçak, Department of Pathology, University of Health Sciences, Sisli Hamidiye Etfal Teaching and Research Hospital, Istanbul, Turkey.
Received: January 22, 2024; Published: September 26, 2024
Citation: Ramazan Uçak., et al. “Ligneous-Cervisitis". Acta Scientific Clinical Case Reports 8.10 (2024):46-49.
Plasminogen deficiency is a very rare multiple system disorder and it is characterized by the development of fibrin-rich pseudomembranes on the mucous membranes, which is defined as ligneous inflammation. Due to its long-term symptoms, ineffective treatment, and primary infertility, it seriously affects patient life. When evaluating clinical and pathological data, it should be considered in differential diagnosis.
Keywords: Plasminogen Deficiency; Primary İnfertility; Ligneous İnflammation
The human plasminogen is a protein molecule consisting of 810-amino acids. It is synthesized primarily in the liver. However, adrenal glands, kidney, brain, testicle, heart, lung, uterus, spleen, thymus and intestine are among the resources [1]. Plasminogen plays an important role in fibrinolysis and wound healing. Plasminogen deficiency is thought to cause fibrin accumulation and the formation of pseudomembranous changes due to the inability of the fibrin to break down [1-4]. It is also functional in cell migration, tissue remodeling, angiogenesis and embryogenesis [1]. Plasminogen deficiency is a very rare multiple system disorder and It is characterized by the development of fibrin-rich pseudomembranes on the mucous membranes, which is defined as ligneous inflammation. It is classified into 2 types. Type 1 is congenital hypoplasminogenemia with autosomal recessive inheritance, plasminogen antigen and activity are decreased. Type 2 is the functional type (dysplasminogenemia), where only plasminogen activity is reduced. [2-6]. In the process that developed between 1847 and 1933 by defining the lesions in the conjunctiva as pseudomembranes, it began to be used as ligneous inflammation since 1933 [7]. It is most commonly seen in conjunctiva [4,8-10]. But, it can affect many systems.These include the female genital system (vagina,cervix,endometrium,ovary,fallopian tube), oral cavity, middle ear, respiratory tract, trachea,larynx, pericard, paranasal sinuses,peritoneum, nose, mouth, kidneys, gastrointestinal tract, anüs, gingiva, parametrial tissues [3,6]. In addition, many cases where female genital tract was affected with conjunctivitis have been reported [11-15].
The case is a 39-year-old primary infertile woman. Implantation has been repeatedly attempted for pregnancy. From the neonatal period, she was exposed to resistant infections of the conjunctiva and oral region (gingiva, tonsilla palatina) and resistant eardrum inflammation. In addition, there are tear drops due to constantly drying eyes, use of prosthesis due to tooth loss due to permanent and ulcerative gingivitis, tonsillectomy due to resistant tonsillitis. Unfortunately, in this process, the possibility of plasminogen deficiency and the development of related lesions was not suspected. And with the process, the problem of infertility has developed. During primary infertility follow-up, pathological findings seen in biopsies taken as a result of various gynecological interventions have been reported. These are summarized below:
In addition, atypical cells were not observed in cervical smears taken at different times. The HPV effect has not been established.
And now, she applied to the clinic with the complaint of irregular bleeding and cervical discharge. In the colposcopic examination, vascularized, hemorrhagic and ulcerated appearance was observed in the cervix (Figure 1). The possibility of malignancy could not be excluded. Biopsy was performed from the cervix and endometrium.

Figure 1: Ectocervix with hemorrhagic, fibrinous, exudative appearance, Colposcopic examination.
Histopathologically, routine Hematoxylin-Eosin preparations of samples taken from the cervix and endometrium were examined. When cervical tissue samples were examined, neutrophil polymorphs and infiltrated endocervical columnar/ectocervical squamous epithelium fragments were seen. There was dense fibrin under the epithelium. The endometrium had the same inflammatory reaction and histomorphology consisting of endometrial stroma/gland fragments, including fibrin aggregates (Figure 2).
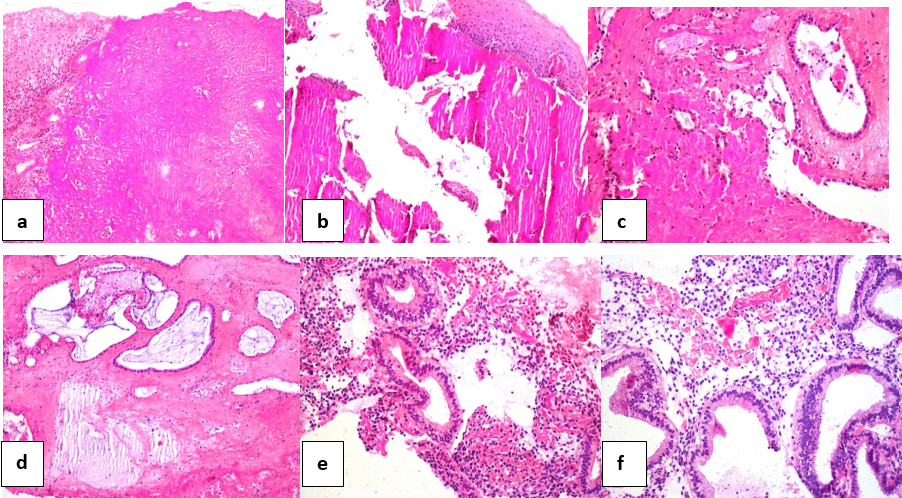
Figure 2: a) Ectoservical squamous epithelium (upper left corner), dense fibrinous material, HE, X100, b) Ectoservical squamous epithelium (upper right corner), fragmente fibrinous material, HE, X100, c) Endoservical glandular tissue (upper), fibrinous material, HE, X100, d) Fibrin and inflammatory cells that integrate with the endocervical glandular tissue, HE, X200, e) Fragmented endometrial stromal-glandular tissue mixed with fibrinous material, HE, X100 f) Endometrial glandular-stromal tissue, fibrinous material (upper), HE, X200.
Ligneous cervicitis/endometritis was considered. Clinically all hematological parameters and plasminogen levels were investigated. Low plasminogen activity level (14% in our case, Normal range 80-120%) was determined. Type I plasminogen deficiency was defined in the case with clinical history, determination of plasminogen deficiency and presence of ligneous cervicitis/endometritis.
Ligneous inflammation of the female genital tract is one of the rare interesting lesions. It may be difficult for the gynecologist or pathologist to think of at the first moment. Therefore, it may be difficult to have a differential diagnosis. As stated in an article [16], gynecologists and most pathologists experienced in gynecology may not be aware of this disease. However, due to the characteristic histology of these lesions, the diagnosis can be made easily when considered [16]. The gynecologist can confuse with inflammatory lesions, the possibility of malignancy (as in our case). The pathologist may not think that there may be a specific inflammatory lesion (in our case, genital tract and tuba biopsies reported as nonspecific inflammation and fibrin aggregates). For these reasons, it is important to know the history of the cases and to collaborate with the pathologist-clinician. To illustrate this confusion, in a case report, microscopic examination of endocervical biopsy, back to back glands with hyperchromatic or vesicular nuclei were considered and microglandular cervical adenocarcinoma was thought. However, this error was avoided by the gynecologist and pathologist working together. And the authors criticized the importance of multidisciplinary work [17]. In a similar case report, atypical changes were observed in cervical biopsy with ligneous inflammation. Clear cell adenocarcinoma may have been thought, but as a result of additional immunohistochemical tests, atypical microglandular hyperplasia has been reported [18]. In many cases, ligneous inflammation in the female genital tract is associated with ligneous conjunctivitis [11,13,15,16,19]. Therefore, these lesions were initially reported as ligneous conjunctivitis and additional genital tract involvement [11-13,20].
In the literature, ligneous inflammation has been reported in 30 cases in the female genital tract. 21 cases confirmed to have type 1 plasminogen deficiency [6]. In 23 (76.7%) of 30 cases, the disease affected multiple organs as in our case. In only 7 women, ligneous lesions only affected the female genital tract. In these cases, the most frequently affected part of the female genital tract is cervix (17/30, 56.7%). Endometrium, ovarian and fallopian tubes are less frequent [6]. Although the cervix and vagina association is common [15,21-23], some cases have spread to vulva and fallopian tubes [24]. In one case, gingiva, paranasal sinus and peritoneal involvement were reported in addition to the female genital tract [25]. In our case, there is an interesting clinical course that starts with conjunctiva in the neonatal period, continues with gingiva, tonsilla palatina, middle ear involvement in childhood, and progresses to the female genital tract in adulthood. Dysmenorrhea, dyspareunia and postcoital bleeding are the leading causes of gynecological symptoms in these cases [6,26-28]. However, they often coexisted with an important problem, such as infertility [6,14,16,17,19,22,23,27,28]. Moreover, it has been suggested that plasminogen deficiency and associated ligneous inflammation can lead to male infertility [29]. Many treatment methods have been tried for symptoms. Adequate treatment has not been found due to the rapid regrowth of membranous lesions after excision [6]. Surgical treatment has a negative effect on the clinical course [30]. It is not only diagnosed, but also difficult to treat [31]. Topical plasmin and plasminogen have been tried in the treatment of ligneous conjunctivitis. Topical plasminogen has been reported to fully dissolve ligneous membranes and is effective for ligneous conjunctivitis [6,31]. Fresh frozen plasma (FFP) infusion is an option to increase plasminogen levels. However, it has its drawbacks and side effects [31].
We present an interesting and rare case involving many systems, multiple organ involvement. Long-term history, clinical and pathological diagnosis difficulties were remarkable factors. It is also difficult to treat. The presence of this disease should be remembered in the female genital tract and lesions manifested by fibrin masses, clinical history should be questioned, especially in terms of eye and oropharyngeal mucosal involvement.
We would like to thank Dr. Nedim Polat for their contribution.
Copyright: © 2024 Ramazan Uçak., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.